Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Hyperaldosteronism Clinical Features Diagnosis and Management Guide
Frequently Asked Questions
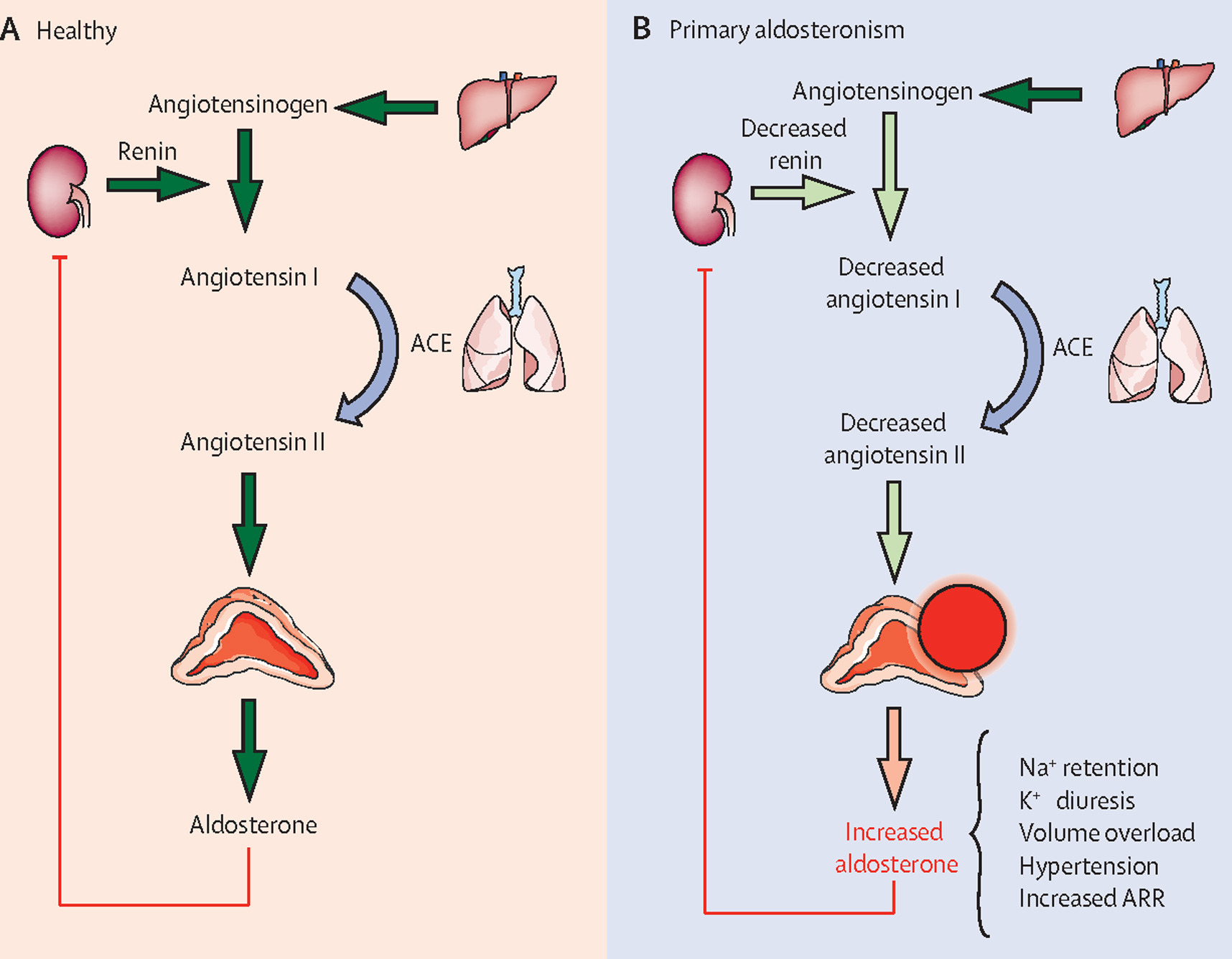
Hyperaldosteronism is a condition characterized by excessive secretion of aldosterone from the adrenal cortex, leading to sodium and water retention, potassium loss, metabolic alkalosis, and hypertension.
The main types are primary hyperaldosteronism (autonomous aldosterone secretion with low renin), secondary hyperaldosteronism (renin-mediated aldosterone excess), and pseudohyperaldosteronism (aldosterone-like effects without high aldosterone).
Primary hyperaldosteronism is caused by autonomous aldosterone production from the adrenal glands, most commonly due to aldosterone-producing adenoma or bilateral adrenal hyperplasia, with suppressed renin levels.
Secondary hyperaldosteronism results from increased renin secretion due to conditions such as renal artery stenosis, heart failure, cirrhosis, nephrotic syndrome, diuretic use, or pregnancy.
Conn syndrome refers to primary hyperaldosteronism caused by an aldosterone-producing adrenal adenoma.
Common features include resistant hypertension, hypokalemia, muscle weakness, fatigue, polyuria, polydipsia, metabolic alkalosis, and increased cardiovascular risk.
No, hypokalemia is not mandatory. Many patients with primary hyperaldosteronism have normal serum potassium levels, especially in early or mild disease.
Screening is recommended in resistant hypertension, hypertension with hypokalemia, adrenal incidentaloma with hypertension, early-onset hypertension, or family history of early stroke or hyperaldosteronism.
The plasma aldosterone–renin ratio (ARR) is the preferred initial screening test.
Confirmation is done using suppression tests such as saline infusion test, oral sodium loading test, fludrocortisone suppression test, or captopril challenge test.
Adrenal venous sampling is the gold standard to differentiate unilateral from bilateral aldosterone secretion and is required before surgical intervention.
Unilateral disease is treated with laparoscopic adrenalectomy, which often normalizes potassium levels and improves or cures hypertension.
Bilateral disease is managed medically using mineralocorticoid receptor antagonists such as spironolactone or eplerenone.
Common drugs include spironolactone, eplerenone, and amiloride, depending on the cause and patient tolerance.
Complications include stroke, myocardial infarction, atrial fibrillation, left ventricular hypertrophy, chronic kidney disease, and increased cardiovascular mortality.
Aldosterone escape occurs due to pressure natriuresis and atrial natriuretic peptide, preventing persistent edema despite sodium retention.
Metabolic alkalosis occurs due to increased hydrogen ion secretion in the renal tubules.
It is a glucocorticoid-remediable form of hyperaldosteronism caused by a genetic defect, where aldosterone secretion is regulated by ACTH and suppressed by low-dose glucocorticoids.
With early diagnosis and appropriate treatment, prognosis is excellent, with significant reduction in cardiovascular and renal complications.
Yes, unilateral primary hyperaldosteronism can often be cured with adrenalectomy, while bilateral disease can be effectively controlled with medical therapy.