Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
High Altitude Pulmonary Edema and Hypothermia Clinical Features Diagnosis and Management
Frequently Asked Questions
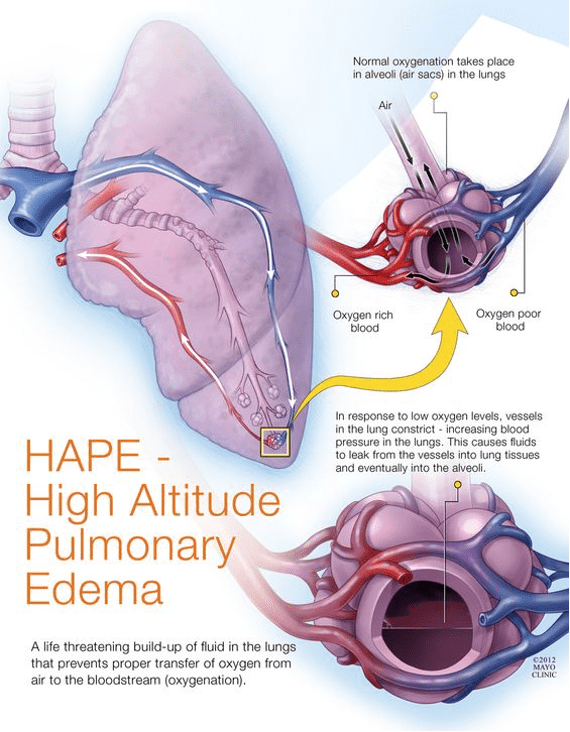
High altitude pulmonary edema is a life-threatening non-cardiogenic pulmonary edema caused by hypoxia-induced pulmonary hypertension after rapid ascent to high altitude, usually above 2500 to 3000 meters.
It is caused by uneven hypoxic pulmonary vasoconstriction leading to high pulmonary artery pressure, capillary stress failure, and leakage of protein-rich fluid into the alveoli.
Early symptoms include reduced exercise tolerance, exertional dyspnea, dry cough, fatigue, and mild chest tightness.
Severe signs include dyspnea at rest, orthopnea, pink frothy sputum, cyanosis, tachycardia, hypoxemia, and bilateral lung crackles.
Diagnosis is primarily clinical based on symptoms, hypoxemia, chest findings, and history of recent ascent, supported by chest X-ray showing patchy bilateral infiltrates with normal heart size.
Immediate descent to a lower altitude combined with supplemental oxygen is the most critical and life-saving treatment.
Nifedipine is the primary drug used; phosphodiesterase-5 inhibitors like sildenafil may be used, and dexamethasone is added if cerebral edema is suspected.
Prevention includes gradual ascent, adequate acclimatization, avoiding strenuous exertion, keeping warm, and prophylactic nifedipine in individuals with prior HAPE.
Hypothermia is a condition in which core body temperature falls below 35 degrees Celsius due to excessive heat loss or impaired thermoregulation.
Hypothermia is classified as mild at 32 to 35 degrees Celsius, moderate at 28 to 32 degrees Celsius, and severe below 28 degrees Celsius.
Common causes include environmental cold exposure, immersion in cold water, high altitude exposure, alcohol or sedative use, sepsis, hypothyroidism, and malnutrition.
Mild hypothermia presents with shivering, tachycardia, slurred speech, impaired coordination, and cold diuresis.
Osborn or J waves on ECG are characteristic of hypothermia and indicate increased risk of ventricular arrhythmias.
Management includes gentle handling, airway and circulation support, correction of hypoglycemia, and rewarming using passive, active external, or active internal methods depending on severity.
The key principle is that no one is considered dead until warm and dead, as hypothermia can mimic death and patients may recover after rewarming.