Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Cushing Syndrome Comprehensive Clinical Guide Diagnosis Causes and Management
Frequently Asked Questions
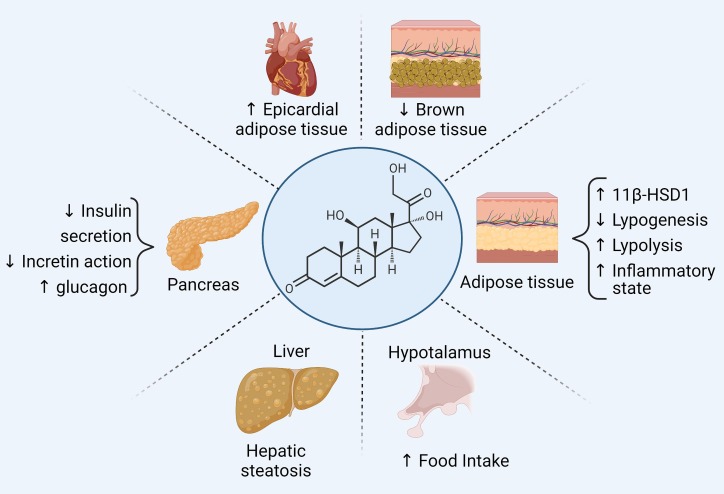
Cushing syndrome is a clinical condition caused by chronic exposure to excess glucocorticoids, either from exogenous steroid use or endogenous overproduction of cortisol.
Cushing syndrome refers to all causes of cortisol excess, while Cushing disease specifically refers to cortisol excess due to an ACTH-secreting pituitary adenoma.
The most common cause of Cushing syndrome is exogenous glucocorticoid therapy.
Classic features include central obesity, moon face, buffalo hump, purple striae, proximal muscle weakness, hypertension, diabetes, osteoporosis, and easy bruising.
Initial screening includes overnight 1 mg dexamethasone suppression test, 24-hour urinary free cortisol, or late-night salivary cortisol measurement.
It detects loss of normal diurnal cortisol rhythm, which is a hallmark of Cushing syndrome.
Plasma ACTH levels are measured; low ACTH suggests ACTH-independent causes, while normal or high ACTH indicates ACTH-dependent Cushing syndrome.
Very high cortisol levels activate mineralocorticoid receptors, leading to potassium loss and metabolic alkalosis.
Inferior petrosal sinus sampling is the gold standard for distinguishing pituitary from ectopic ACTH secretion.
Transsphenoidal surgical removal of the pituitary adenoma is the definitive treatment.
Medical therapy is used when surgery is contraindicated, as a bridge to surgery, or in persistent or recurrent disease.
Ketoconazole, metyrapone, and osilodrostat reduce cortisol synthesis by inhibiting adrenal steroidogenesis enzymes.
Gradual tapering prevents adrenal crisis due to hypothalamic-pituitary-adrenal axis suppression.
Complications include cardiovascular disease, diabetes, osteoporosis, infections, psychiatric disorders, and increased mortality.
Cardiovascular disease is the leading cause of mortality in patients with Cushing syndrome.