Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Percutaneous Coronary Intervention PCI Procedure Indications Risks And Management
Frequently Asked Questions
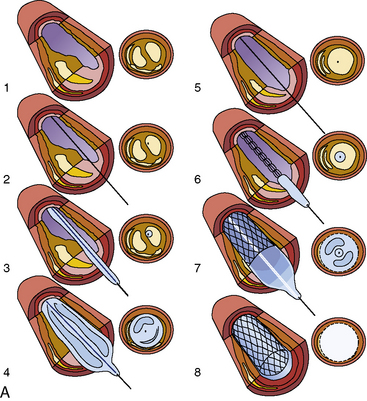
Percutaneous coronary intervention is a minimally invasive cardiac procedure used to open narrowed or blocked coronary arteries using a catheter-based approach, usually involving balloon angioplasty and stent placement to restore myocardial blood flow.
PCI is most strongly indicated in acute ST-elevation myocardial infarction (STEMI), high-risk non-ST elevation acute coronary syndromes, and in patients with refractory angina despite optimal medical therapy.
Coronary angiography is a diagnostic procedure used to visualize coronary arteries, whereas PCI is a therapeutic intervention performed to treat significant coronary artery stenosis identified during angiography.
Drug-eluting stents are coronary stents coated with antiproliferative drugs such as sirolimus or everolimus that reduce neointimal hyperplasia and significantly lower the risk of in-stent restenosis.
Dual antiplatelet therapy consists of aspirin plus a P2Y12 inhibitor such as clopidogrel, ticagrelor, or prasugrel, used to prevent stent thrombosis following PCI.
After drug-eluting stent implantation, DAPT is recommended for at least 12 months in acute coronary syndrome and at least 6 months in stable coronary artery disease, unless bleeding risk dictates otherwise.
Common complications include bleeding at the access site, contrast-induced nephropathy, coronary artery dissection or perforation, acute stent thrombosis, arrhythmias, and in-stent restenosis.
Radial artery access is preferred because it significantly reduces bleeding and vascular complications, allows early ambulation, and improves overall patient comfort compared to femoral access.
PCI provides a clear survival benefit in acute coronary syndromes, especially STEMI, but in stable coronary artery disease it mainly improves symptoms and quality of life rather than long-term mortality.
Premature discontinuation of dual antiplatelet therapy, stent under-expansion, high thrombus burden, diabetes mellitus, renal failure, and complex coronary lesions significantly increase the risk of stent thrombosis.
MCQ Test - Percutaneous Coronary Intervention PCI Procedure Indications Risks And Management
No MCQs available for this article.