Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Hypothyroidism Complete Guide Causes Symptoms Diagnosis and Treatment
Frequently Asked Questions
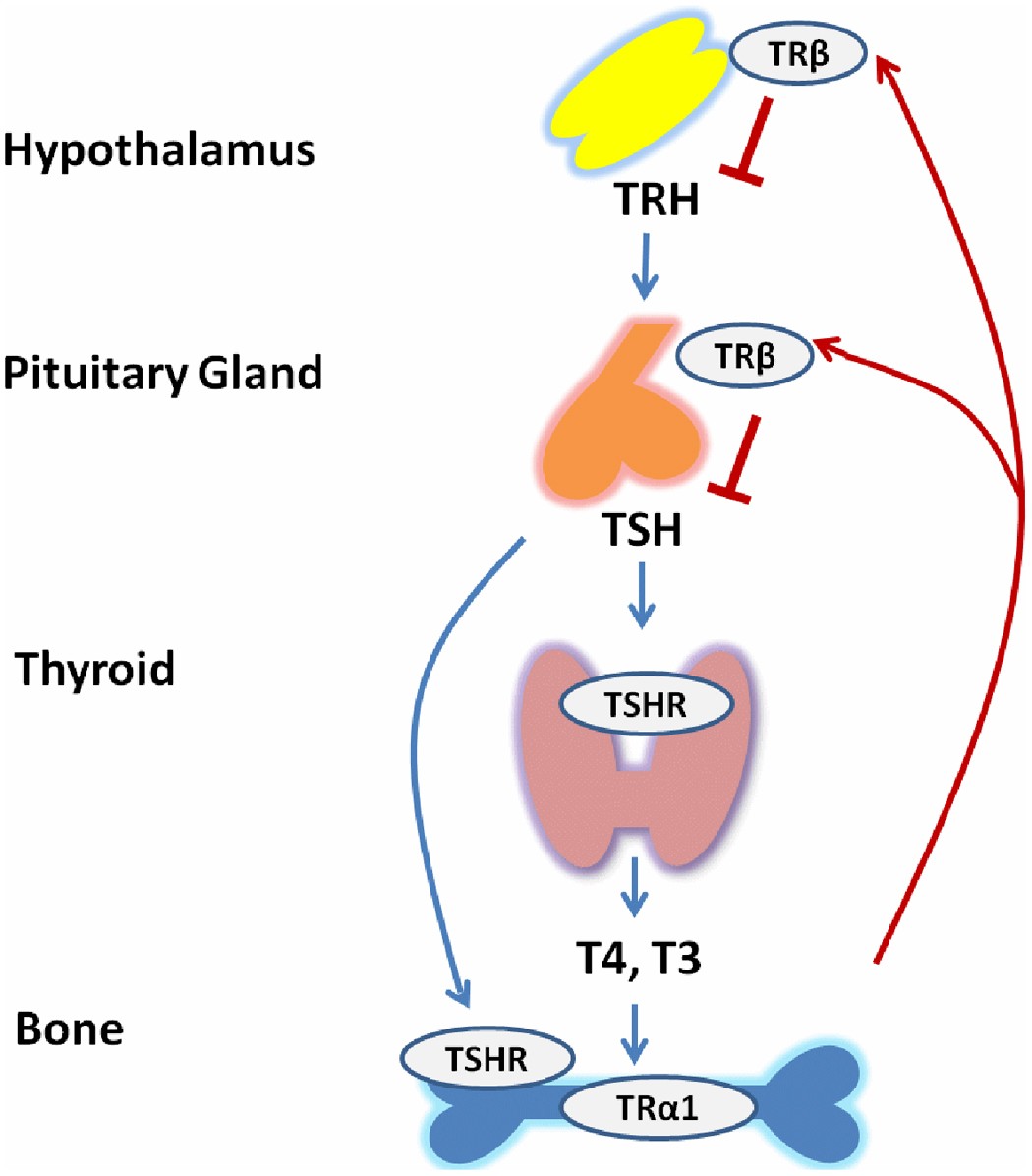
Hypothyroidism is a condition in which the thyroid gland produces insufficient amounts of thyroid hormones (T4 and T3), leading to a generalized slowing of metabolic processes in the body.
The most common cause is Hashimoto thyroiditis, an autoimmune disorder in which antibodies destroy thyroid tissue.
Common symptoms include fatigue, cold intolerance, weight gain, constipation, dry skin, hair loss, depression, bradycardia, and menstrual irregularities.
Diagnosis is primarily made by laboratory testing showing elevated TSH with low free T4 in primary hypothyroidism.
Subclinical hypothyroidism is defined by elevated TSH levels with normal free T4 levels, often with mild or no symptoms.
Treatment is recommended when TSH is greater than 10 mIU/L, in symptomatic patients, during pregnancy, or when anti-TPO antibodies are positive.
Levothyroxine (synthetic T4) is the treatment of choice and is usually required lifelong in primary hypothyroidism.
Levothyroxine should be taken orally on an empty stomach, preferably in the morning, 30–60 minutes before food, and separated from calcium or iron supplements by at least 4 hours.
TSH levels are monitored every 6–8 weeks after starting or adjusting therapy, and once stable, every 6–12 months.
In secondary hypothyroidism, pituitary dysfunction leads to inappropriately normal or low TSH, so free T4 is used for monitoring.
Complications include hyperlipidemia, cardiovascular disease, infertility, anemia, hyponatremia, and myxedema coma.
Myxedema coma is a life-threatening complication of severe hypothyroidism characterized by hypothermia, altered mental status, bradycardia, and respiratory failure.
Steroids are given to prevent precipitating adrenal crisis due to possible coexisting adrenal insufficiency.
Yes, untreated hypothyroidism increases the risk of miscarriage, preeclampsia, and impaired fetal neurodevelopment.
In most cases, especially autoimmune hypothyroidism, it is lifelong and requires continuous thyroid hormone replacement.