Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
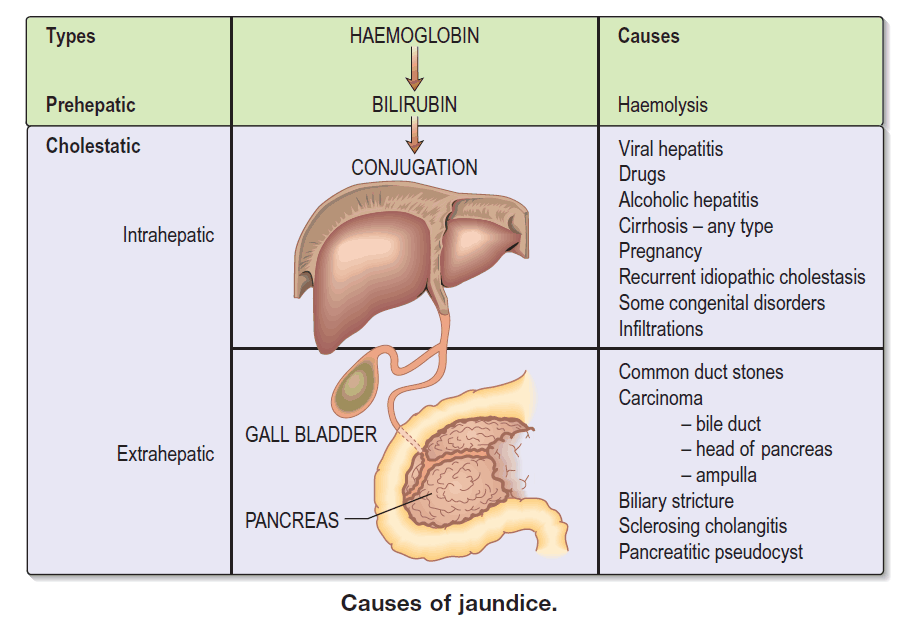
Differential Diagnosis of Jaundice Complete Causes Types Clinical Approach
Frequently Asked Questions
Jaundice is yellow discoloration of the skin, sclera, and mucous membranes caused by elevated serum bilirubin levels, usually above 2–3 mg/dL.
The three main types are prehepatic (hemolytic), hepatic (hepatocellular), and posthepatic (obstructive or cholestatic) jaundice.
Prehepatic jaundice is caused by excessive breakdown of red blood cells, leading to unconjugated hyperbilirubinemia, commonly due to hemolytic anemia.
Hepatic jaundice results from liver cell dysfunction due to hepatitis, cirrhosis, drug-induced liver injury, alcohol-related liver disease, or metabolic disorders.
Posthepatic jaundice is caused by obstruction of bile flow due to gallstones, pancreatic cancer, bile duct strictures, or cholangiocarcinoma.
Unconjugated jaundice is usually due to hemolysis or genetic disorders, while conjugated jaundice is associated with bile obstruction or liver excretory dysfunction.
Key tests include total and direct bilirubin, ALT, AST, ALP, GGT, complete blood count, reticulocyte count, viral hepatitis markers, and coagulation profile.
Pale stools, dark urine, severe itching, elevated ALP and GGT, and progressive painless jaundice suggest obstructive jaundice.
Anemia, splenomegaly, elevated reticulocyte count, unconjugated hyperbilirubinemia, and absence of bilirubin in urine suggest hemolytic jaundice.
Red flag causes include acute liver failure, pancreatic cancer, cholangiocarcinoma, biliary atresia in infants, severe drug toxicity, and sepsis.
Pale or clay-colored stools indicate biliary obstruction, while normal-colored stools suggest non-obstructive jaundice.
Ultrasound abdomen is first-line, followed by MRCP, CT scan, or ERCP when obstruction or malignancy is suspected.
Genetic causes include Gilbert syndrome, Crigler–Najjar syndrome, Dubin–Johnson syndrome, Rotor syndrome, Wilson disease, and alpha-1 antitrypsin deficiency.
Neonatal jaundice may be physiologic or caused by hemolysis, infection, biliary atresia, metabolic disorders, or genetic bilirubin conjugation defects.
Alcohol damages hepatocytes, impairs bilirubin metabolism, and causes alcoholic hepatitis or cirrhosis leading to hepatic jaundice.
Sepsis can cause cholestasis due to impaired bile excretion, resulting in conjugated hyperbilirubinemia.
Painless progressive jaundice is commonly associated with pancreatic cancer or cholangiocarcinoma.
The first step is to determine whether hyperbilirubinemia is conjugated or unconjugated and assess liver enzyme patterns.
Marked elevation of ALP and GGT compared to ALT and AST suggests cholestatic or obstructive jaundice.
Jaundice can indicate life-threatening conditions such as acute liver failure, malignancy, severe infection, or major biliary obstruction, requiring urgent evaluation.