Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Hyperthyroidism Clinical Guide Diagnosis Causes Symptoms Treatment
Frequently Asked Questions
Hyperthyroidism is a clinical condition caused by excessive production and release of thyroid hormones (T3 and T4) from the thyroid gland, leading to a hypermetabolic state.
Hyperthyroidism refers specifically to increased hormone production by the thyroid gland, whereas thyrotoxicosis refers to excess circulating thyroid hormones from any cause, including exogenous intake or thyroiditis.
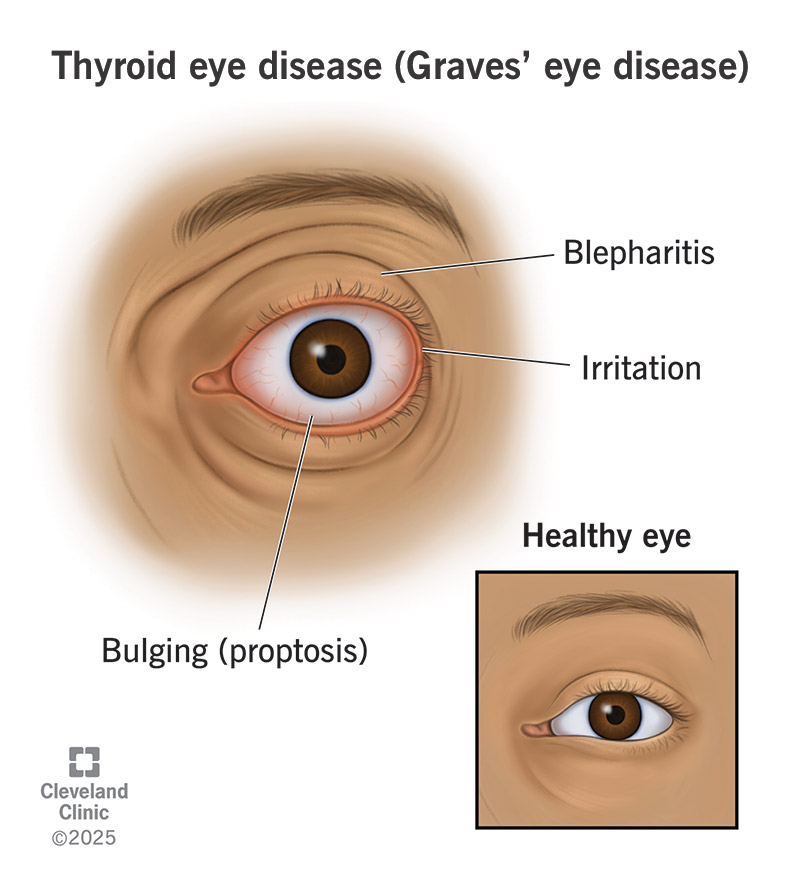
Graves’ disease is the most common cause of hyperthyroidism worldwide, especially in young and middle-aged women.
Weight loss despite increased appetite, heat intolerance, palpitations, tremors, anxiety, excessive sweating, and fatigue are cardinal symptoms.
Excess thyroid hormones increase beta-adrenergic receptor sensitivity, leading to tachycardia, increased cardiac output, and palpitations.
Suppressed TSH with elevated free T4 and/or free T3 levels is the hallmark laboratory finding.
T3 toxicosis is a form of hyperthyroidism where TSH is suppressed and T3 is elevated while T4 remains within the normal range.
Apathetic hyperthyroidism is a presentation seen mainly in elderly patients, characterized by weight loss, depression, atrial fibrillation, and minimal adrenergic symptoms.
Graves’ disease is diagnosed by clinical features, suppressed TSH, elevated thyroid hormones, positive TSH receptor antibodies, and diffuse increased uptake on radioactive iodine scan.
In thyroiditis, excess hormones are released from damaged follicles rather than newly synthesized, resulting in low radioactive iodine uptake.
Treatment options include beta-blockers for symptom control, antithyroid drugs (methimazole or propylthiouracil), radioactive iodine therapy, and surgery.
Beta-blockers control adrenergic symptoms such as tremors, palpitations, and anxiety; propranolol also reduces peripheral conversion of T4 to T3.
Agranulocytosis is the most serious adverse effect, presenting with fever and sore throat and requiring immediate drug cessation.
Propylthiouracil is preferred in the first trimester due to lower teratogenic risk compared to methimazole.
Thyroid storm is a life-threatening complication of severe hyperthyroidism characterized by hyperpyrexia, delirium, severe tachycardia, and heart failure.
Iodine is given after antithyroid drugs to prevent stimulation of new hormone synthesis and to block hormone release.
Atrial fibrillation, high-output heart failure, widened pulse pressure, and worsening angina are common cardiovascular complications.
Yes, excess thyroid hormones increase bone resorption, leading to decreased bone mineral density and osteoporosis.
Subclinical hyperthyroidism is defined by suppressed TSH with normal T3 and T4 levels and may still increase cardiovascular and bone risks.
Most patients develop permanent hypothyroidism and require lifelong levothyroxine replacement.