Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Depression Treatment Guide Symptoms Causes Therapy Medications and Recovery
Frequently Asked Questions
Depression is a mental health disorder characterized by persistent sadness, loss of interest, fatigue, poor concentration, sleep disturbances, and reduced daily functioning lasting at least two weeks.
Symptoms include low mood, loss of interest, hopelessness, guilt, fatigue, appetite changes, sleep problems, poor concentration, and suicidal thoughts.
Depression can be caused by genetic factors, brain chemical imbalance, stressful life events, trauma, chronic illness, substance use, and hormonal changes.
Depression is diagnosed through clinical interviews, symptom duration assessment, psychiatric evaluation, and standardized screening tools based on DSM-5 criteria.
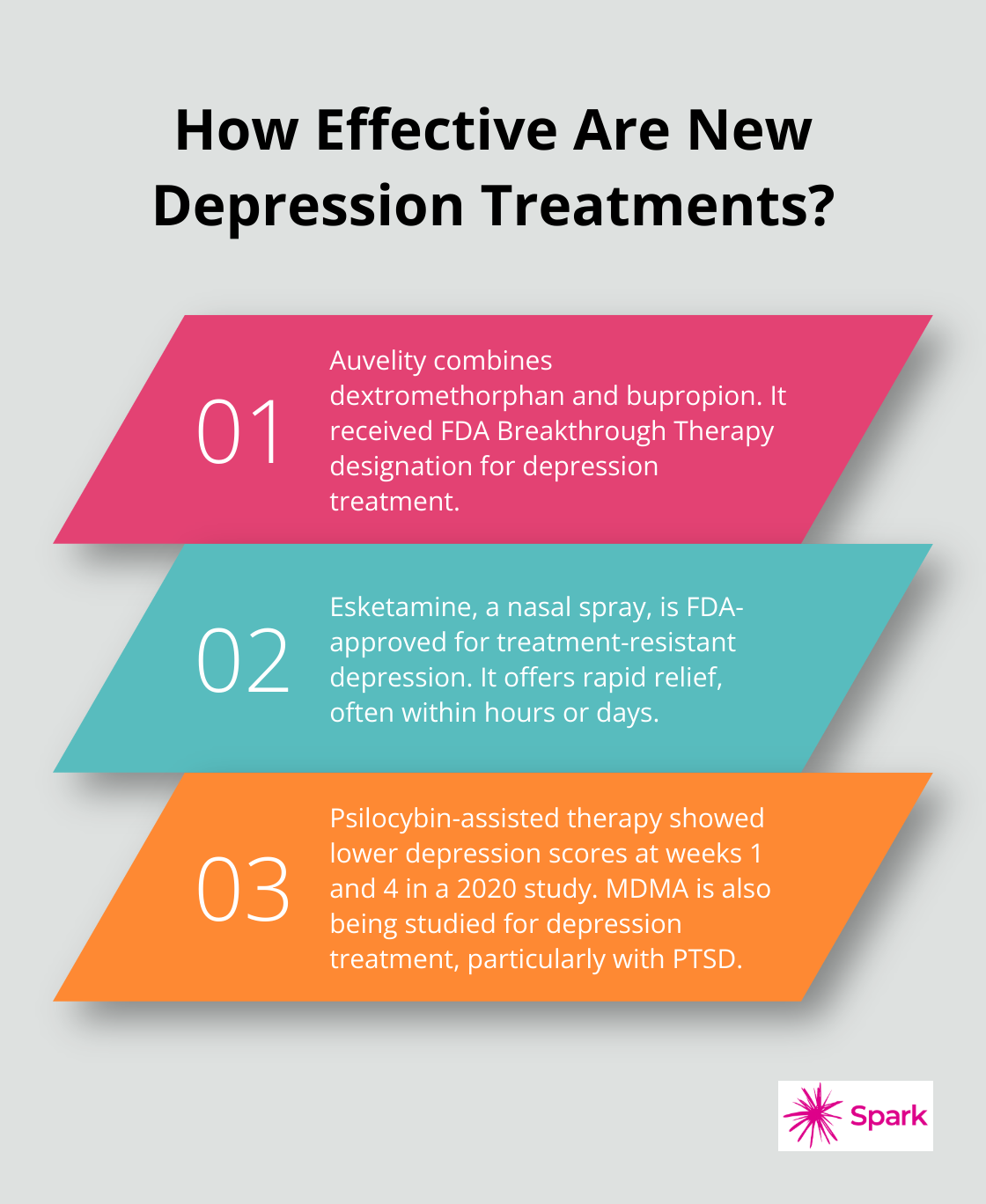
Treatment includes psychotherapy, antidepressant medications, lifestyle changes, social support, and advanced therapies like ECT or TMS in severe cases.
Common antidepressants include SSRIs, SNRIs, bupropion, mirtazapine, tricyclic antidepressants, and MAO inhibitors depending on patient response.
Most antidepressants take 2 to 6 weeks to show noticeable improvement, with full benefits often seen by 8 to 12 weeks.
Yes, mild to moderate depression can often be managed with psychotherapy, lifestyle changes, exercise, sleep improvement, and stress management.
Treatment-resistant depression refers to depression that does not respond to at least two adequate trials of antidepressant medications.
ECT is used in severe, psychotic, suicidal, or medication-resistant depression where rapid symptom improvement is needed.
Yes, untreated depression significantly increases the risk of suicidal thoughts, suicide attempts, and self-harm.
Treatment should continue for at least 6 to 12 months after symptom remission, and longer in recurrent cases.
Depression is highly treatable, and many patients achieve full remission with proper medical and psychological care.
Regular exercise, good sleep, healthy diet, stress management, social engagement, avoiding alcohol, and structured daily routines support recovery.
Warning signs include persistent suicidal thoughts, inability to function, psychotic symptoms, severe withdrawal, and refusal to eat or drink.
Yes, depression affects children and adolescents, often presenting with irritability, academic decline, social withdrawal, and self-harm behavior.
Depression can relapse, especially if treatment is stopped early, but long-term therapy and lifestyle management reduce recurrence.
Sadness is temporary, while depression is persistent, more severe, affects daily life, and lasts for weeks or months.
Risk can be reduced through stress management, emotional support, healthy lifestyle, early intervention, and mental health awareness.
Professional help should be sought if symptoms last more than two weeks, worsen over time, interfere with daily life, or involve suicidal thoughts.