Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Edema Causes Symptoms Diagnosis and Complete Medical Management
Frequently Asked Questions
Edema is the abnormal accumulation of fluid in the interstitial tissues, leading to visible or palpable swelling of body parts.
Edema is caused by increased capillary hydrostatic pressure, decreased plasma oncotic pressure, increased capillary permeability, lymphatic obstruction, and renal sodium and water retention.
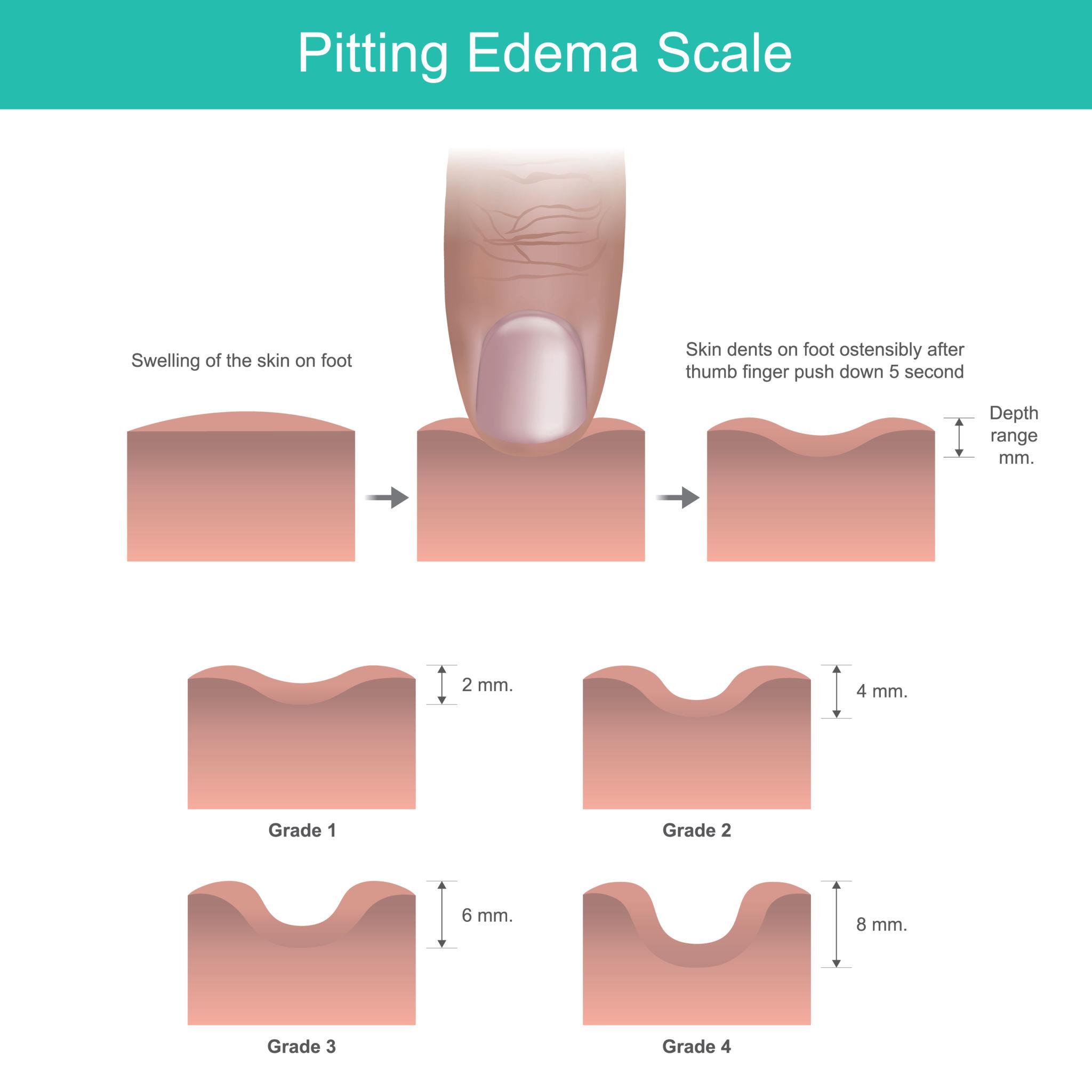
Pitting edema leaves a persistent indentation when pressure is applied and is seen in cardiac, renal, and hepatic causes, while non-pitting edema does not pit and occurs in lymphedema and myxedema.
Nephrotic syndrome causes massive protein loss in urine leading to hypoalbuminemia, reduced plasma oncotic pressure, and fluid shift into interstitial spaces.
In heart failure, prolonged standing increases venous pressure in dependent areas, leading to fluid accumulation that worsens by evening.
Deposition of glycosaminoglycans in the interstitial tissue leads to water retention, resulting in non-pitting edema called myxedema.
Anasarca refers to severe, generalized edema involving the entire body, often seen in advanced heart failure, nephrotic syndrome, or liver cirrhosis.
Common drugs causing edema include calcium channel blockers, NSAIDs, corticosteroids, and thiazolidinediones.
Clinical evaluation includes assessing pitting, distribution, timing of swelling, associated symptoms, and systemic signs such as raised JVP, proteinuria, or ascites.
Management includes treating the underlying cause, salt and fluid restriction, limb elevation, compression therapy when appropriate, and diuretics when indicated.