Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
Symptomatic Bradycardia With Pulse Management Guidelines and Drug Dosing
Frequently Asked Questions
Symptomatic bradycardia with a pulse is a clinical condition where the heart rate is abnormally slow, usually below 60 beats per minute, and the patient has a palpable pulse but develops symptoms such as hypotension, syncope, dizziness, altered mental status, chest pain, or signs of shock due to reduced cardiac output.
There is no absolute heart rate cutoff, but rates below 50 beats per minute, and especially below 40 beats per minute, are more likely to cause symptoms and hemodynamic instability, particularly in elderly patients or those with structural heart disease.
Common causes include sinus node dysfunction, high-grade atrioventricular block, myocardial ischemia or infarction, drug effects such as beta-blockers or calcium channel blockers, electrolyte abnormalities like hyperkalemia, hypothyroidism, hypoxia, hypothermia, and increased vagal tone.
Diagnosis is based on clinical symptoms combined with ECG findings showing bradyarrhythmia. Continuous cardiac monitoring, 12-lead ECG, blood pressure measurement, and evaluation for reversible causes are essential.
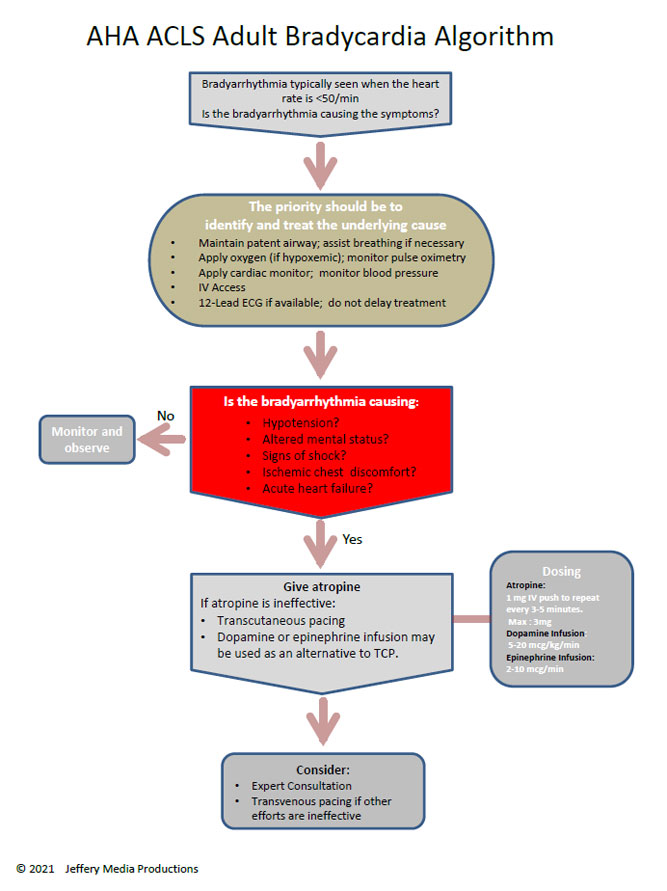
Symptoms of unstable bradycardia include hypotension, acute altered mental status, ischemic chest discomfort, syncope, signs of shock, and acute heart failure.
Atropine given intravenously is the first-line medication for most cases of symptomatic bradycardia with a pulse, unless contraindicated or ineffective due to high-grade conduction block.
Atropine is often ineffective in Mobitz type II atrioventricular block, complete heart block, and bradycardia due to infranodal conduction disease or severe hypothermia.
Transcutaneous pacing is indicated in patients with symptomatic bradycardia who are hemodynamically unstable and do not respond to atropine or when atropine is contraindicated or unlikely to be effective.
Dopamine or epinephrine intravenous infusions may be used as temporary measures to increase heart rate and blood pressure when pacing is unavailable or while preparing for pacing.
Management includes stopping the offending drug, providing supportive care, administering atropine if symptomatic, and using specific antidotes or advanced therapies in cases of overdose.
Electrolyte disturbances, especially hyperkalemia, can cause severe bradycardia and conduction blocks. Correction of the electrolyte abnormality is the definitive treatment.
No, bradycardia can be physiological, such as in well-trained athletes or during sleep, and does not require treatment unless symptoms or hemodynamic compromise are present.
A permanent pacemaker is indicated in patients with symptomatic sinus node dysfunction, Mobitz type II atrioventricular block, complete heart block, or recurrent symptomatic bradycardia not due to reversible causes.
Investigations include continuous ECG monitoring, serum electrolytes, renal function tests, thyroid function tests, cardiac biomarkers if ischemia is suspected, and echocardiography to assess structural heart disease.
Yes, recurrence is common if the underlying cause is not corrected, which is why definitive treatment such as pacemaker implantation may be necessary in recurrent or persistent cases.