Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
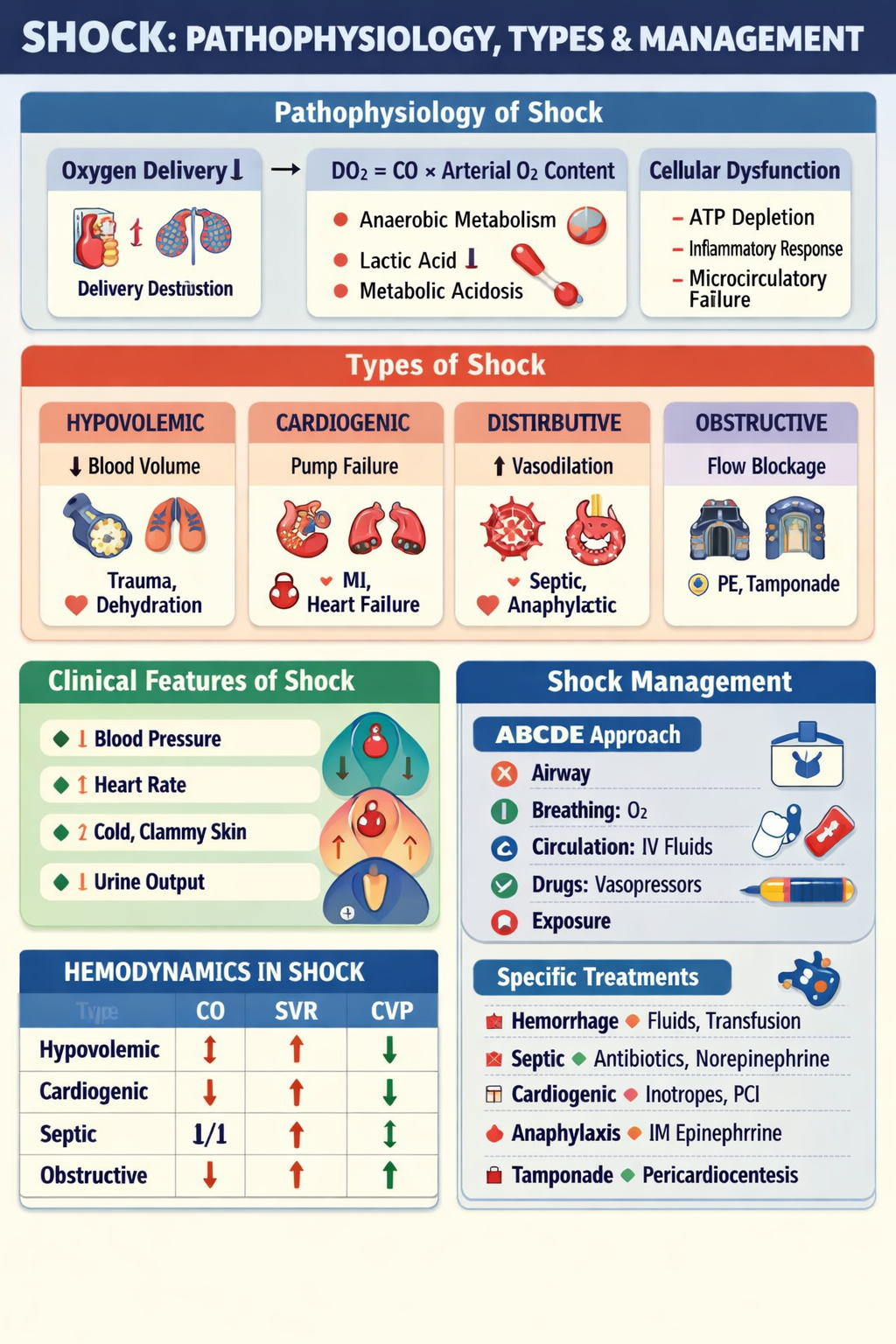
Shock Pathophysiology Types and Emergency Management Guide
Frequently Asked Questions
Shock is a life-threatening condition where tissue perfusion and oxygen delivery are inadequate, leading to cellular hypoxia, metabolic acidosis, and organ dysfunction.
Shock occurs due to failure of oxygen delivery to tissues, causing anaerobic metabolism, lactic acidosis, ATP depletion, inflammatory mediator release, microcirculatory dysfunction, and eventually multi-organ failure.
The major types of shock are hypovolemic shock, cardiogenic shock, distributive shock (septic, anaphylactic, neurogenic), and obstructive shock.
Hypovolemic shock is caused by severe loss of intravascular volume due to hemorrhage, dehydration, burns, vomiting, diarrhea, or plasma loss.
Cardiogenic shock results from pump failure of the heart, leading to reduced cardiac output despite adequate volume, commonly due to myocardial infarction, arrhythmias, myocarditis, or severe heart failure.
Septic shock causes systemic vasodilation due to cytokine and nitric oxide release, along with capillary leak and myocardial depression, resulting in reduced systemic vascular resistance and hypotension.
Neurogenic shock is characterized by hypotension with bradycardia and warm dry skin due to loss of sympathetic tone, usually after spinal cord injury.
Obstructive shock is caused by mechanical obstruction to blood flow, such as pulmonary embolism, cardiac tamponade, or tension pneumothorax.
Early signs include tachycardia, anxiety, cold extremities, delayed capillary refill, mild hypotension or normal blood pressure, and reduced urine output.
Elevated serum lactate is a key marker of tissue hypoperfusion and anaerobic metabolism in shock.
The first step is immediate ABCDE resuscitation: secure airway, provide high-flow oxygen, establish IV access, start fluid resuscitation, and treat the underlying cause.
Crystalloids such as normal saline or Ringer lactate are first-line for initial fluid resuscitation in most shock types.
Norepinephrine is the first-line vasopressor used in septic shock to maintain mean arterial pressure above 65 mmHg.
Immediate intramuscular epinephrine is the life-saving first-line treatment for anaphylactic shock, followed by airway support and adjunct therapies.
Cardiogenic shock requires inotropes and revascularization, and excessive fluids are avoided due to risk of pulmonary edema, whereas hypovolemic shock requires aggressive fluid and blood replacement.
Shock progresses through compensated stage (tachycardia, vasoconstriction), progressive stage (hypotension, organ dysfunction), and irreversible stage (refractory multi-organ failure).
Key endpoints include MAP ≥65 mmHg, urine output ≥0.5 mL/kg/hr, improving mental status, lactate clearance, and normalization of perfusion signs.
Untreated shock can lead to multi-organ failure, disseminated intravascular coagulation, ARDS, irreversible tissue damage, and death.