Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Pulseless Electrical Activity Clinical Features Diagnosis and Management Guide
Frequently Asked Questions
Pulseless electrical activity is a cardiac arrest rhythm in which organized electrical activity is seen on ECG but there is no palpable pulse or effective cardiac output.
No, pulseless electrical activity is a non-shockable rhythm and should not be treated with defibrillation.
Death in PEA occurs due to failure of mechanical cardiac contraction despite preserved electrical activity, leading to complete circulatory collapse.
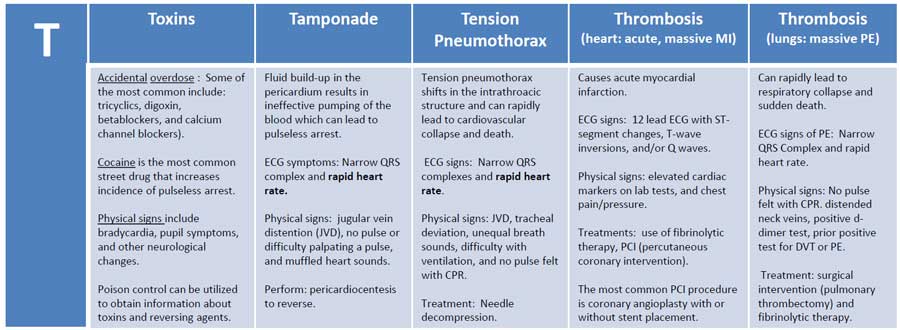
The common reversible causes are summarized as Hs and Ts, including hypovolemia, hypoxia, acidosis, hypo- or hyperkalemia, hypothermia, tension pneumothorax, cardiac tamponade, toxins, thrombosis (coronary or pulmonary), and trauma.
Immediate high-quality CPR along with early administration of intravenous or intraosseous epinephrine and rapid identification of reversible causes.
The recommended adult dose is 1 mg IV or IO every 3–5 minutes during resuscitation.
Defibrillation is ineffective because PEA does not involve chaotic electrical activity but rather a failure of mechanical contraction.
Pseudo-PEA refers to organized electrical activity with minimal cardiac contraction detectable only by ultrasound, without a palpable pulse.
Bedside ultrasound helps identify reversible causes such as cardiac tamponade, massive pulmonary embolism, severe hypovolemia, and distinguishes true PEA from pseudo-PEA.
Severe hyperkalemia is a frequent and life-threatening cause of PEA in patients with renal failure.
End-tidal CO2 monitoring helps assess CPR quality and prognosis, with persistently low values indicating poor perfusion and low chance of ROSC.
PEA generally has a poorer prognosis than ventricular fibrillation or pulseless ventricular tachycardia, especially if no reversible cause is identified.
Yes, massive myocardial infarction or mechanical complications such as ventricular rupture can lead to PEA.
The most important principle is rapid identification and correction of reversible causes while continuing high-quality CPR.
Termination is considered when prolonged high-quality resuscitation fails to achieve ROSC and no reversible causes are identified, following institutional and ethical guidelines.