Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
First Heart Sound S1 and Jugular Venous Pulse JVP Clinical Examination Guide
Frequently Asked Questions
The first heart sound (S1) is produced by the closure of the atrioventricular valves—mitral (M1) and tricuspid (T1)—at the beginning of ventricular systole during the isovolumetric contraction phase.
The mitral component (M1) contributes most to S1 and is best heard at the cardiac apex.
A loud S1 is caused by a short PR interval, mobile mitral valve leaflets (as in mitral stenosis), hyperdynamic circulation (fever, anemia, thyrotoxicosis), and thin chest wall.
A soft S1 occurs due to long PR interval, mitral regurgitation, calcified mitral valve, left ventricular failure, obesity, or emphysema.
In atrial fibrillation, the PR interval varies beat to beat, leading to variable timing of AV valve closure and hence variable intensity of S1.
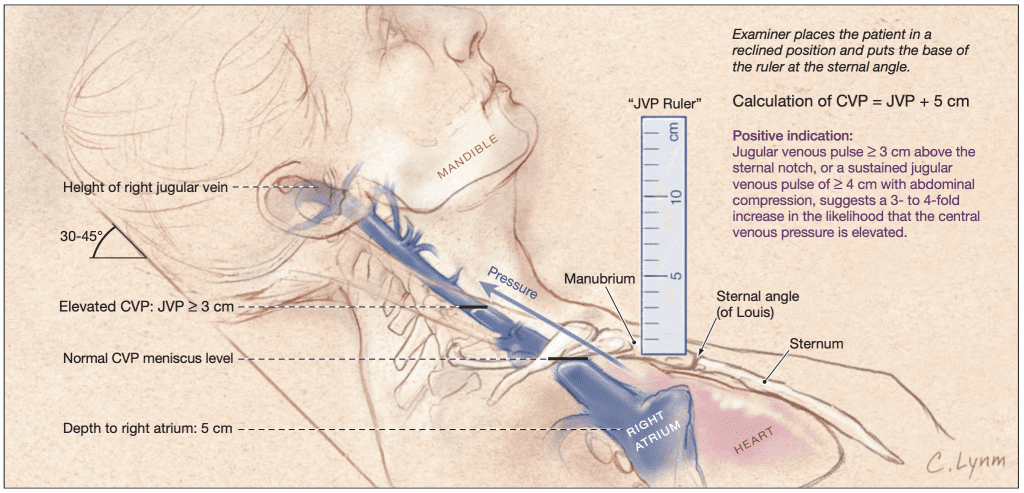
The jugular venous pulse is the visible pulsation of the internal jugular vein reflecting right atrial pressure and right heart hemodynamics.
The internal jugular vein has a direct connection to the right atrium, lacks valves, and accurately reflects central venous pressure.
The normal JVP waveform consists of a wave (atrial contraction), c wave (tricuspid bulging), x descent (atrial relaxation), v wave (venous filling), and y descent (ventricular filling).
A raised JVP indicates elevated right atrial pressure and is seen in right heart failure, tricuspid valve disease, constrictive pericarditis, cardiac tamponade, pulmonary hypertension, and fluid overload.
Absent a waves are seen in atrial fibrillation due to the absence of organized atrial contraction.
Cannon a waves are large intermittent a waves caused by atrial contraction against a closed tricuspid valve, seen in complete heart block and other AV dissociation states.
Prominent v waves are characteristic of tricuspid regurgitation due to systolic backflow of blood into the right atrium.
Kussmaul’s sign is a paradoxical rise in JVP during inspiration, seen in constrictive pericarditis, restrictive cardiomyopathy, and right ventricular infarction.
In cardiac tamponade, JVP is raised with a prominent x descent and an absent y descent due to impaired ventricular filling.
Combined assessment of S1 and JVP helps in diagnosing valvular heart disease, arrhythmias, right heart failure, and pericardial disorders at the bedside.