Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
Infective Endocarditis Clinical Features Diagnosis and Management Guide
Frequently Asked Questions
Infective endocarditis is a microbial infection of the endocardial surface of the heart, most commonly involving the heart valves, characterized by vegetation formation, systemic embolization, and immune-mediated complications.
The most common organisms are Staphylococcus aureus, viridans streptococci, Enterococci, coagulase-negative staphylococci (especially in prosthetic valves), and HACEK organisms.
Major risk factors include prosthetic heart valves, previous infective endocarditis, congenital heart disease, rheumatic or degenerative valve disease, intravenous drug use, indwelling catheters, and immunosuppression.
Common features include fever, new or changing heart murmur, embolic phenomena, vascular signs such as Janeway lesions, immunologic signs such as Osler nodes and glomerulonephritis, and systemic manifestations like weight loss and fatigue.
Janeway lesions are painless erythematous lesions on palms and soles caused by septic emboli, while Osler nodes are painful nodules on fingers or toes due to immune complex deposition.
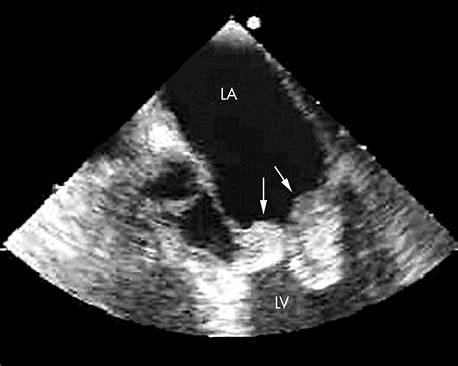
Essential investigations include multiple blood cultures before antibiotics, echocardiography (TTE followed by TEE if needed), inflammatory markers, urine analysis, and imaging for embolic complications.
TEE has higher sensitivity than transthoracic echocardiography, especially for detecting vegetations on prosthetic valves, periannular abscesses, and small lesions.
The modified Duke criteria are used to establish the diagnosis of infective endocarditis based on a combination of clinical, microbiological, and echocardiographic findings.
Culture-negative infective endocarditis refers to cases where blood cultures are negative, commonly due to prior antibiotic use or infection with fastidious organisms such as Coxiella burnetii or Bartonella species.
Intravenous antibiotic therapy is typically required for 4 to 6 weeks for native valve endocarditis and at least 6 weeks for prosthetic valve endocarditis.
Combination therapy is used to achieve bactericidal synergy, particularly in enterococcal endocarditis and prosthetic valve infections.
Indications include acute heart failure due to valve dysfunction, uncontrolled infection, periannular abscess, recurrent embolization, large vegetations, and prosthetic valve dehiscence.
Complications include heart failure, stroke, systemic embolization, renal failure, conduction abnormalities, mycotic aneurysms, and death.
Injection of contaminated material introduces bacteria directly into the venous circulation, commonly infecting the tricuspid valve.
Antibiotic prophylaxis is recommended only for high-risk patients undergoing certain dental procedures to prevent bacteremia-induced endocarditis.