Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Rheumatic Heart Disease Clinical Features Diagnosis Management and Prevention
Frequently Asked Questions
Rheumatic heart disease is a chronic valvular heart condition caused by immune-mediated damage following acute rheumatic fever, which occurs after untreated or inadequately treated Group A streptococcal throat infection.
The mitral valve is most commonly affected, followed by the aortic valve. Tricuspid involvement is usually secondary, and pulmonary valve involvement is rare.
Acute rheumatic fever causes an autoimmune reaction due to molecular mimicry between streptococcal antigens and cardiac tissue, leading to inflammation, fibrosis, and permanent valvular damage.
Common symptoms include exertional dyspnea, orthopnea, paroxysmal nocturnal dyspnea, hemoptysis, palpitations due to atrial fibrillation, and thromboembolic events such as stroke.
Left atrial enlargement due to mitral stenosis or regurgitation predisposes to atrial fibrillation, increasing the risk of thromboembolism.
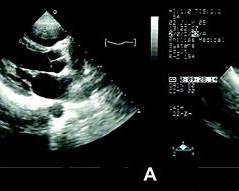
Echocardiography is the gold standard investigation as it defines valve morphology, severity of stenosis or regurgitation, chamber sizes, pulmonary pressures, and complications like atrial thrombus.
Secondary prophylaxis with long-acting benzathine penicillin prevents recurrent streptococcal infections and recurrent rheumatic fever, thereby slowing progression of valvular damage.
Duration depends on severity: at least 5 years or until age 21 without carditis, 10 years or until age 21 with carditis, and often lifelong in patients with residual valvular disease.
It is indicated in symptomatic severe rheumatic mitral stenosis with favorable valve anatomy and absence of left atrial thrombus or significant mitral regurgitation.
Warfarin is preferred because clinical trials have shown inferior protection with direct oral anticoagulants in rheumatic mitral stenosis.
Complications include atrial fibrillation, thromboembolism, infective endocarditis, pulmonary hypertension, heart failure, stroke, and sudden cardiac death.
Pregnancy increases blood volume and heart rate, which can precipitate pulmonary edema and heart failure, especially in mitral stenosis.
Ortner syndrome refers to hoarseness of voice due to compression of the left recurrent laryngeal nerve by an enlarged left atrium in severe mitral stenosis.
Valve surgery is indicated in severe symptomatic valvular disease, presence of left ventricular dysfunction, or when percutaneous intervention is not suitable.
Prevention includes early treatment of streptococcal pharyngitis, long-term secondary prophylaxis after rheumatic fever, improved living conditions, and access to primary healthcare.