Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
Aortic Regurgitation Comprehensive Guide Causes Symptoms Diagnosis Treatment
Frequently Asked Questions
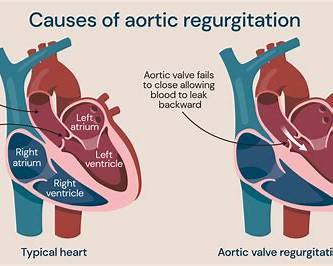
Aortic regurgitation is a valvular heart disease in which blood flows back from the aorta into the left ventricle during diastole due to incomplete closure of the aortic valve.
Common causes include bicuspid aortic valve, rheumatic heart disease, infective endocarditis, aortic root dilation, Marfan syndrome, aortic dissection, and degenerative valve disease.
Acute aortic regurgitation develops suddenly and causes severe pulmonary edema and hypotension, while chronic aortic regurgitation progresses slowly with left ventricular dilation and a long asymptomatic phase.
Symptoms include exertional dyspnea, fatigue, palpitations, angina, orthopnea, and paroxysmal nocturnal dyspnea, usually appearing late in the disease.
Wide pulse pressure occurs due to increased systolic pressure from high stroke volume and decreased diastolic pressure from rapid blood runoff back into the left ventricle.
A high-pitched, early diastolic decrescendo murmur best heard along the left sternal border with the patient sitting forward.
Austin Flint murmur is a low-pitched mid-diastolic murmur at the apex caused by the regurgitant aortic jet interfering with mitral valve opening in severe aortic regurgitation.
Echocardiography is the key investigation as it identifies the cause, grades severity, assesses left ventricular size and function, and evaluates the aorta.
Holodiastolic flow reversal in the descending aorta is a hallmark finding of severe aortic regurgitation.
Surgery is indicated when left ventricular ejection fraction is 55 percent or less, LV end-systolic dimension exceeds 50 mm, or indexed LVESD is greater than 25 mm per square meter.
The left ventricle cannot adapt to sudden volume overload, leading to rapid pulmonary edema, cardiogenic shock, and high mortality without urgent valve replacement.
Afterload-reducing agents such as ACE inhibitors, ARBs, and dihydropyridine calcium channel blockers are useful, especially in patients with hypertension or heart failure.
Intra-aortic balloon pump increases diastolic pressure and worsens regurgitant flow back into the left ventricle.
Cardiac MRI is used when echocardiographic assessment is inconclusive, providing accurate measurement of regurgitant volume, regurgitant fraction, and ventricular volumes.
Complications include irreversible left ventricular dysfunction, heart failure, arrhythmias, pulmonary hypertension, infective endocarditis, and increased mortality.