Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
Ischemic Heart Disease Comprehensive Clinical Guide Diagnosis Management and Prevention
Frequently Asked Questions
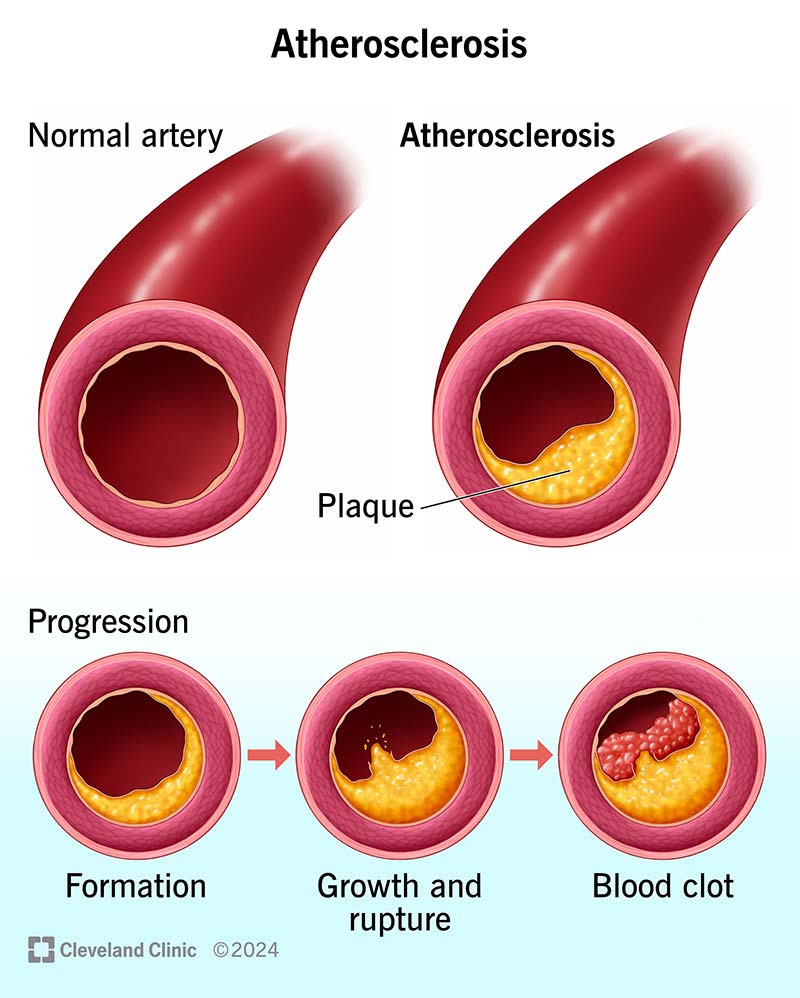
Ischemic heart disease is a condition caused by reduced blood supply to the heart muscle due to narrowing or blockage of coronary arteries, most commonly from atherosclerosis.
The main causes include coronary atherosclerosis, plaque rupture with thrombosis, coronary artery spasm, and microvascular dysfunction. Risk factors include smoking, diabetes, hypertension, dyslipidemia, and obesity.
Typical symptoms include chest pain or pressure, exertional angina, shortness of breath, fatigue, diaphoresis, and in some cases silent ischemia especially in diabetics and elderly patients.
Stable angina occurs predictably with exertion and is relieved by rest or nitrates, while unstable angina occurs at rest or with minimal exertion and indicates a high risk of myocardial infarction.
Diagnosis includes ECG, cardiac biomarkers (troponin), stress testing, echocardiography, coronary CT angiography, and invasive coronary angiography when indicated.
Acute coronary syndrome refers to a spectrum of conditions caused by acute myocardial ischemia, including unstable angina, NSTEMI, and STEMI.
STEMI shows ST-segment elevation on ECG due to complete coronary occlusion, while NSTEMI shows ischemic ECG changes without ST elevation and partial coronary occlusion.
Immediate treatment includes aspirin, ECG monitoring, cardiac biomarkers, anti-ischemic therapy, and rapid assessment for reperfusion strategy.
Primary percutaneous coronary intervention is preferred if it can be performed within guideline-recommended time; otherwise fibrinolytic therapy is used when PCI is not promptly available.
Common medications include antiplatelets (aspirin, P2Y12 inhibitors), statins, beta-blockers, ACE inhibitors or ARBs, nitrates, and anticoagulants in selected cases.
Dual antiplatelet therapy consists of aspirin plus a P2Y12 inhibitor and is used after ACS or PCI to prevent stent thrombosis and recurrent ischemic events.
In most ACS patients, dual antiplatelet therapy is recommended for at least 12 months unless there is a high bleeding risk.
Statins reduce LDL cholesterol, stabilize atherosclerotic plaques, reduce inflammation, and significantly lower the risk of future cardiovascular events.
CABG is preferred in patients with left main disease, triple-vessel disease especially in diabetics, and in those with reduced left ventricular function.
Complications include heart failure, arrhythmias, mechanical complications like papillary muscle rupture, ventricular septal rupture, sudden cardiac death, and ischemic cardiomyopathy.
Ischemic cardiomyopathy is chronic left ventricular dysfunction resulting from repeated or extensive myocardial ischemia or infarction.
Smoking cessation, regular physical activity, heart-healthy diet, weight control, blood pressure control, diabetes management, and stress reduction are essential.
Yes, especially in diabetics and elderly patients, ischemia may occur without chest pain and is known as silent ischemia.
Prognosis depends on extent of coronary disease, left ventricular function, timely reperfusion, adherence to medical therapy, and lifestyle modification.
Cardiac rehabilitation improves exercise tolerance, reduces mortality, enhances quality of life, and promotes long-term adherence to lifestyle and medical therapy.