Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Congestive Heart Failure Comprehensive Guide Diagnosis Classification and Management
Frequently Asked Questions
Congestive heart failure is a clinical syndrome in which the heart is unable to pump sufficient blood to meet the metabolic demands of the body or can do so only at elevated filling pressures, leading to pulmonary and or systemic congestion.
The main types are heart failure with reduced ejection fraction (HFrEF), heart failure with preserved ejection fraction (HFpEF), and heart failure with mildly reduced ejection fraction (HFmrEF).
Common causes include ischemic heart disease, long standing hypertension, valvular heart disease, cardiomyopathies, arrhythmias, and congenital heart disease.
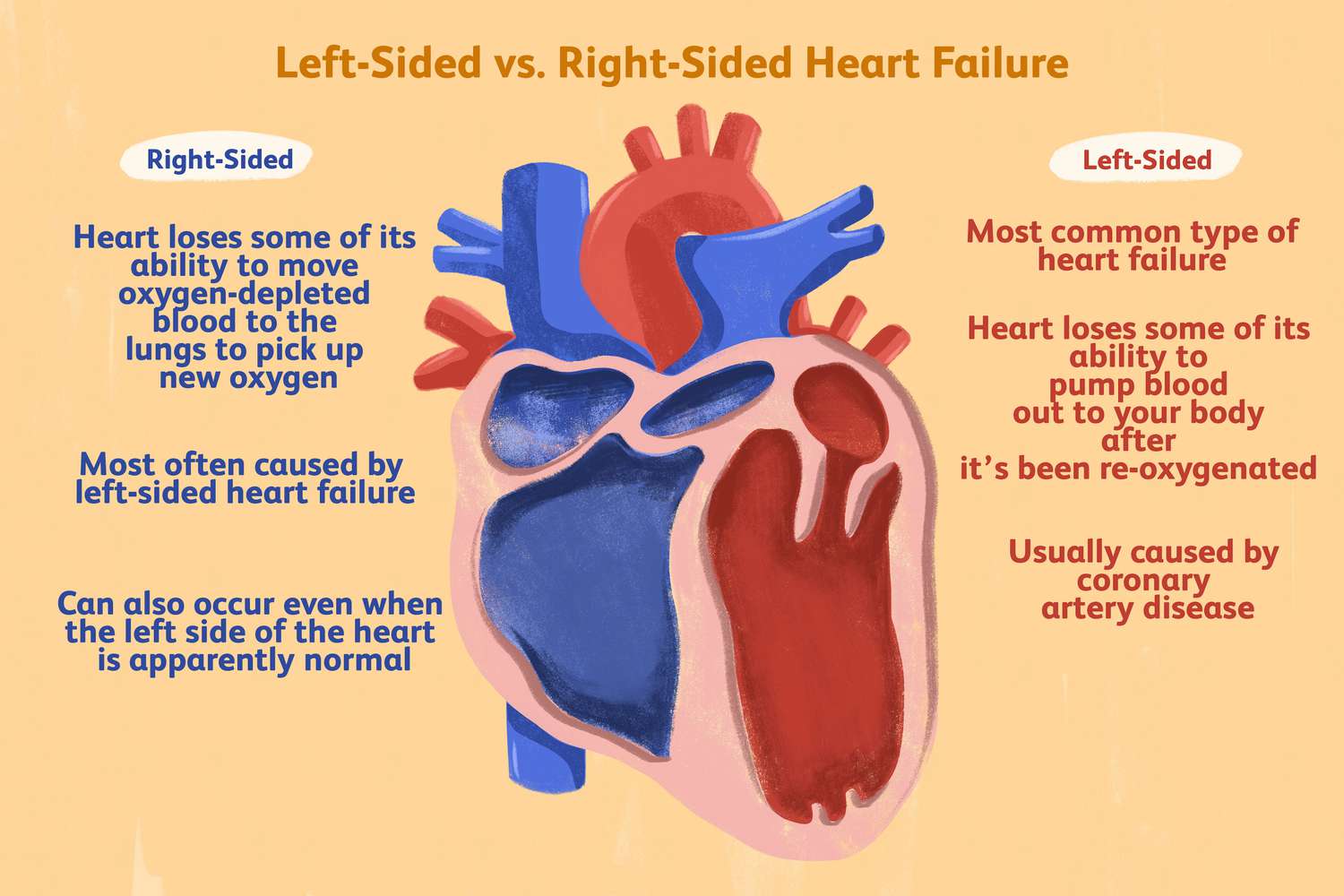
Left sided heart failure commonly presents with dyspnea on exertion, orthopnea, paroxysmal nocturnal dyspnea, cough, and pulmonary edema.
Right sided heart failure presents with raised jugular venous pressure, hepatomegaly, ascites, peripheral edema, and abdominal discomfort.
Key investigations include echocardiography to assess ejection fraction, BNP or NT-proBNP levels, ECG, chest X-ray, renal function tests, electrolytes, and complete blood count.
BNP and NT-proBNP are markers of myocardial stretch; normal levels make heart failure unlikely, while elevated levels support the diagnosis and help assess severity.
Guideline directed medical therapy includes ACE inhibitors or ARNI, evidence based beta blockers, mineralocorticoid receptor antagonists, SGLT2 inhibitors, and diuretics for symptom control.
Diuretics provide symptomatic relief by reducing congestion but do not independently reduce mortality in heart failure.
Beta blockers reduce sympathetic overactivity, prevent arrhythmias, reverse remodeling, and significantly reduce mortality and hospitalization in HFrEF.
Acute decompensated heart failure is a sudden worsening of chronic or new onset heart failure characterized by pulmonary edema, volume overload, or low cardiac output.
Common precipitants include infection, myocardial infarction, uncontrolled hypertension, arrhythmias, renal failure, excess salt intake, and non compliance with medications.
Management of HFpEF focuses on blood pressure control, diuretics for congestion, treatment of atrial fibrillation, and management of comorbidities such as diabetes and obesity.
An ICD is indicated in patients with LVEF 35 percent or less despite optimal medical therapy to prevent sudden cardiac death.
Key lifestyle measures include salt restriction, fluid restriction, daily weight monitoring, smoking cessation, limited alcohol intake, regular physical activity, and vaccination.