Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
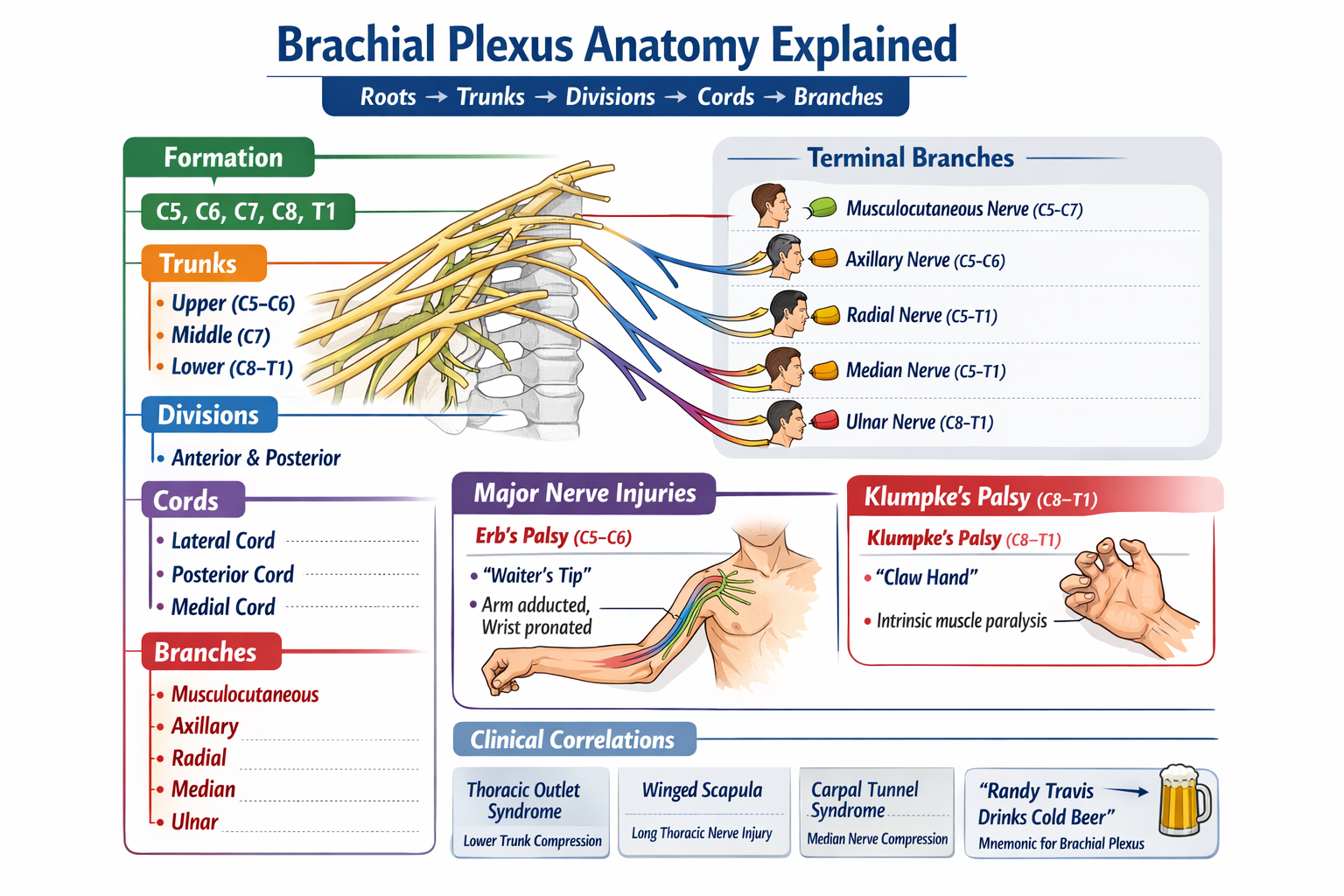
Brachial Plexus Anatomy Explained with Roots Trunks Cords Branches and Clinical Correlations
Frequently Asked Questions
The brachial plexus is a network of ventral rami of spinal nerves C5 to T1 that provides motor, sensory, and sympathetic innervation to the upper limb.
The brachial plexus is formed by the ventral rami of C5, C6, C7, C8, and T1 spinal nerves.
The correct order is Roots, Trunks, Divisions, Cords, and Branches.
There are three trunks: upper trunk (C5–C6), middle trunk (C7), and lower trunk (C8–T1).
Anterior divisions supply flexor compartments of the upper limb, while posterior divisions supply extensor compartments.
They are named according to their position relative to the second part of the axillary artery.
The long thoracic nerve causes winged scapula when injured because it supplies the serratus anterior muscle.
Erb palsy is an upper trunk injury involving C5–C6 nerve roots, resulting in a waiter’s tip deformity.
Klumpke palsy is a lower trunk injury (C8–T1) characterized by intrinsic hand muscle paralysis, claw hand, and sometimes Horner syndrome.
The median nerve receives fibers from all roots C5 to T1.
The musculocutaneous nerve pierces the coracobrachialis muscle.
Radial nerve injury causes wrist drop due to paralysis of wrist extensors.
Thoracic outlet syndrome involves compression of the lower trunk of the brachial plexus as it passes between the clavicle and first rib.
The ulnar nerve arises from the medial cord of the brachial plexus.
It is crucial because injuries at different levels produce characteristic motor and sensory deficits, aiding localization of nerve damage.
MCQ Test - Brachial Plexus Anatomy Explained with Roots Trunks Cords Branches and Clinical Correlations
No MCQs available for this article.