Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Complications of Third Stage of Labour Causes Risks Prevention and Management
Frequently Asked Questions
What is the third stage of labour?
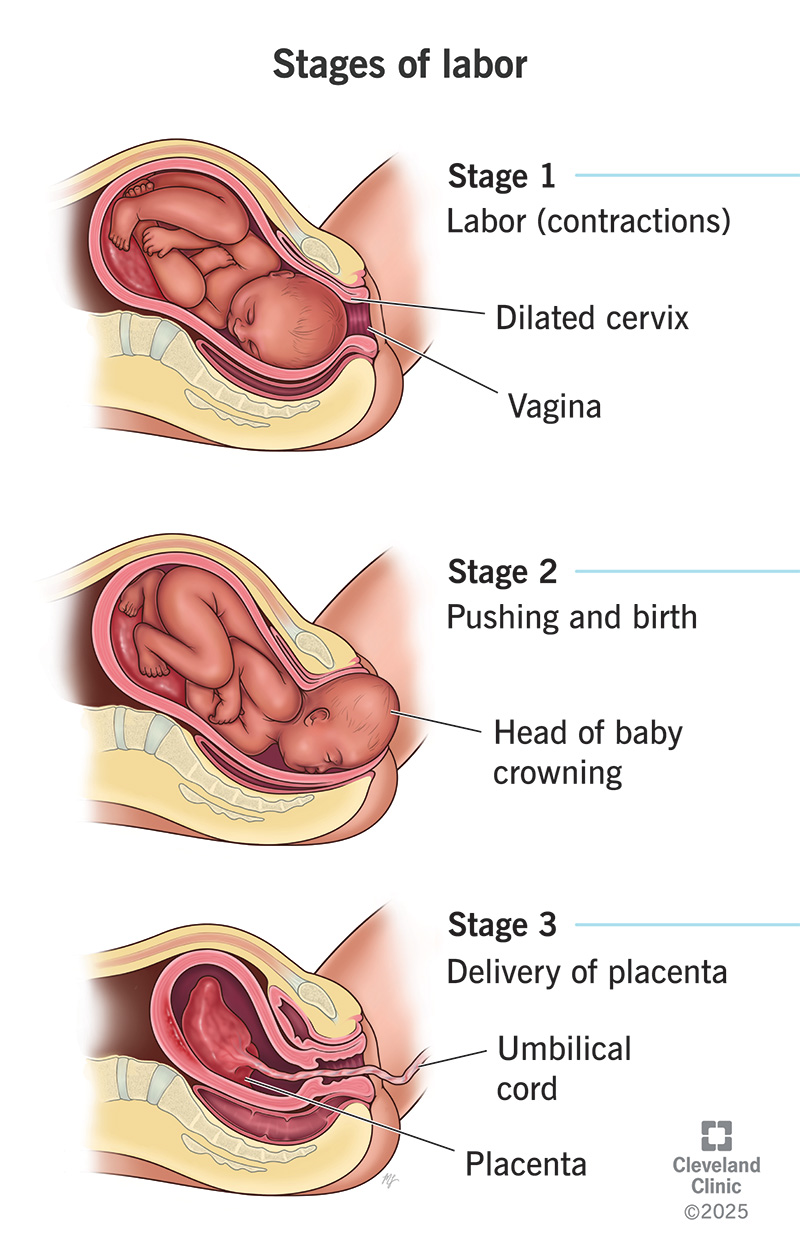
The third stage of labour is the period from the birth of the baby until the complete expulsion of the placenta and membranes.
What is the most common complication of the third stage of labour?
Postpartum hemorrhage due to uterine atony is the most common and most serious complication.
What are the main causes of postpartum hemorrhage in the third stage?
The main causes are described by the 4 Ts: Tone (uterine atony) Tissue (retained placenta) Trauma (genital tract injury) Thrombin (coagulation disorders)
How does placenta accreta cause complications?
Placenta accreta prevents normal placental separation, leading to massive hemorrhage and often requiring surgical intervention or hysterectomy.
How can complications of the third stage of labour be prevented?
Most complications can be prevented by active management of the third stage of labour, skilled birth attendance, and early identification of high-risk cases.
MCQ Test - Complications of Third Stage of Labour Causes Risks Prevention and Management
Progress:
0/30
Time: 00:00
Test Results
0%
0/30
0
Correct Answers
0
Wrong Answers
00:00
Time Taken
0
Skipped