Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
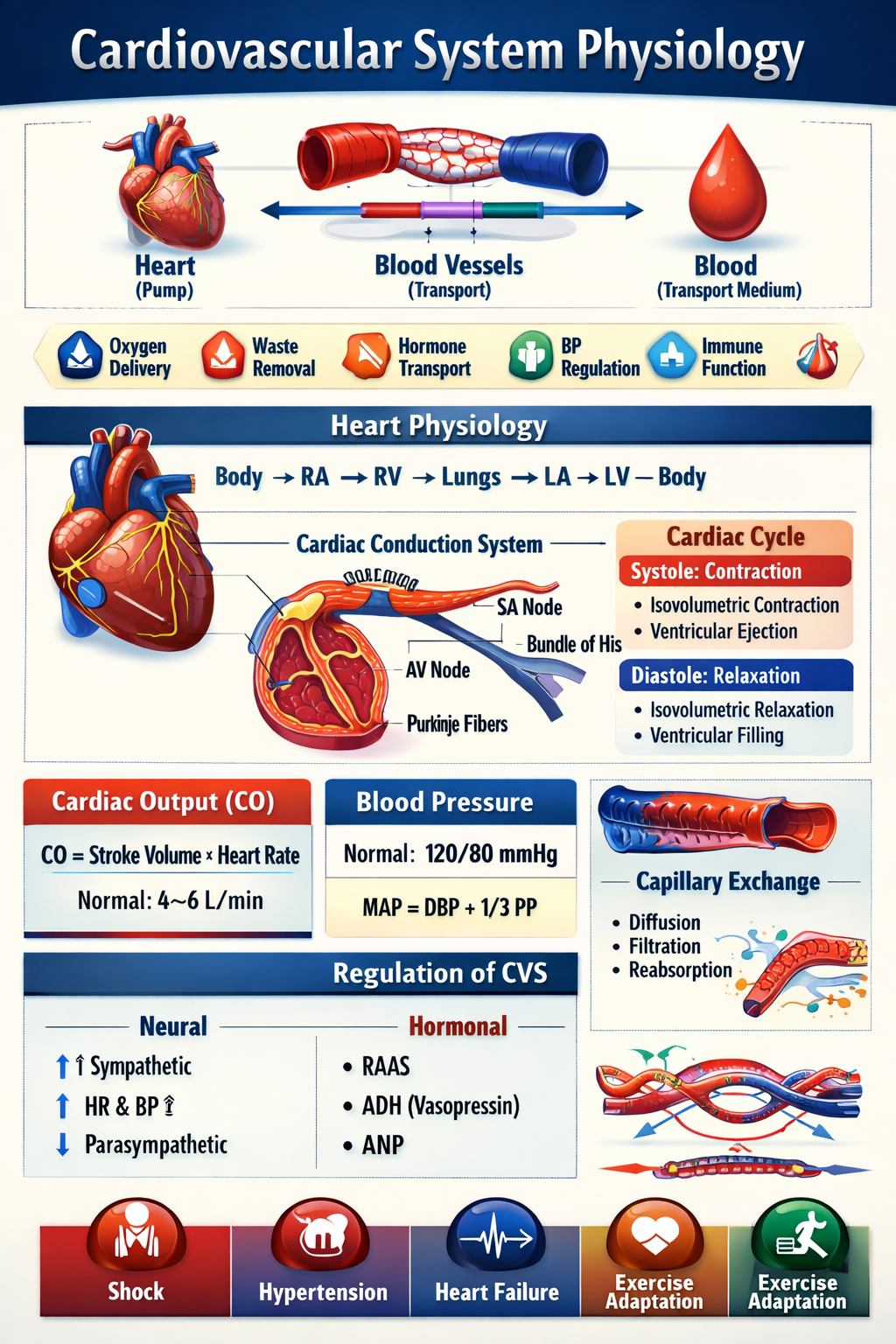
Cardiovascular System Physiology Complete Detailed Guide for Medical Students
Frequently Asked Questions
The cardiovascular system delivers oxygen and nutrients to tissues, removes carbon dioxide and waste products, maintains blood pressure, regulates temperature, and supports homeostasis.
Cardiac output is the volume of blood pumped by the heart per minute and is calculated as stroke volume multiplied by heart rate.
Stroke volume is determined by preload, afterload, myocardial contractility, and ventricular compliance.
The Frank–Starling law states that an increase in venous return leads to increased ventricular filling and stronger myocardial contraction, increasing stroke volume.
Heart rate is controlled by the sinoatrial node and modulated by autonomic nervous system activity, hormones, and reflexes.
The cardiac conduction system generates and transmits electrical impulses to coordinate atrial and ventricular contractions.
Systolic pressure is produced by ventricular contraction, while diastolic pressure reflects arterial recoil and peripheral resistance.
Mean arterial pressure is the average pressure in arteries during one cardiac cycle and ensures adequate organ perfusion.
Arterioles are resistance vessels that regulate peripheral vascular resistance and control blood pressure.
Baroreceptors detect changes in arterial pressure and adjust heart rate and vascular tone via autonomic pathways.
Venous return depends on skeletal muscle pump, respiratory pump, venous valves, and sympathetic venoconstriction.
Capillary exchange involves diffusion, filtration, and reabsorption of fluids and solutes regulated by Starling forces.
Coronary circulation supplies oxygenated blood to the myocardium, primarily occurring during diastole.
Exercise increases heart rate, stroke volume, cardiac output, and redistributes blood flow to active muscles.
Shock results from inadequate tissue perfusion due to reduced cardiac output, low blood volume, or decreased vascular resistance.
Pulse pressure widens due to increased stroke volume or reduced arterial compliance, such as in aortic regurgitation.
Pulmonary circulation carries deoxygenated blood to the lungs for gas exchange and returns oxygenated blood to the heart.
Left ventricular hypertrophy occurs due to chronic pressure overload, such as hypertension or aortic stenosis.
Aging reduces arterial elasticity, increases blood pressure, decreases cardiac reserve, and slows reflex responses.
The refractory period prevents tetanic contraction and ensures rhythmic and coordinated cardiac contractions.