Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Neonatal Jaundice Detailed Guide Causes Symptoms Diagnosis Treatment
Frequently Asked Questions
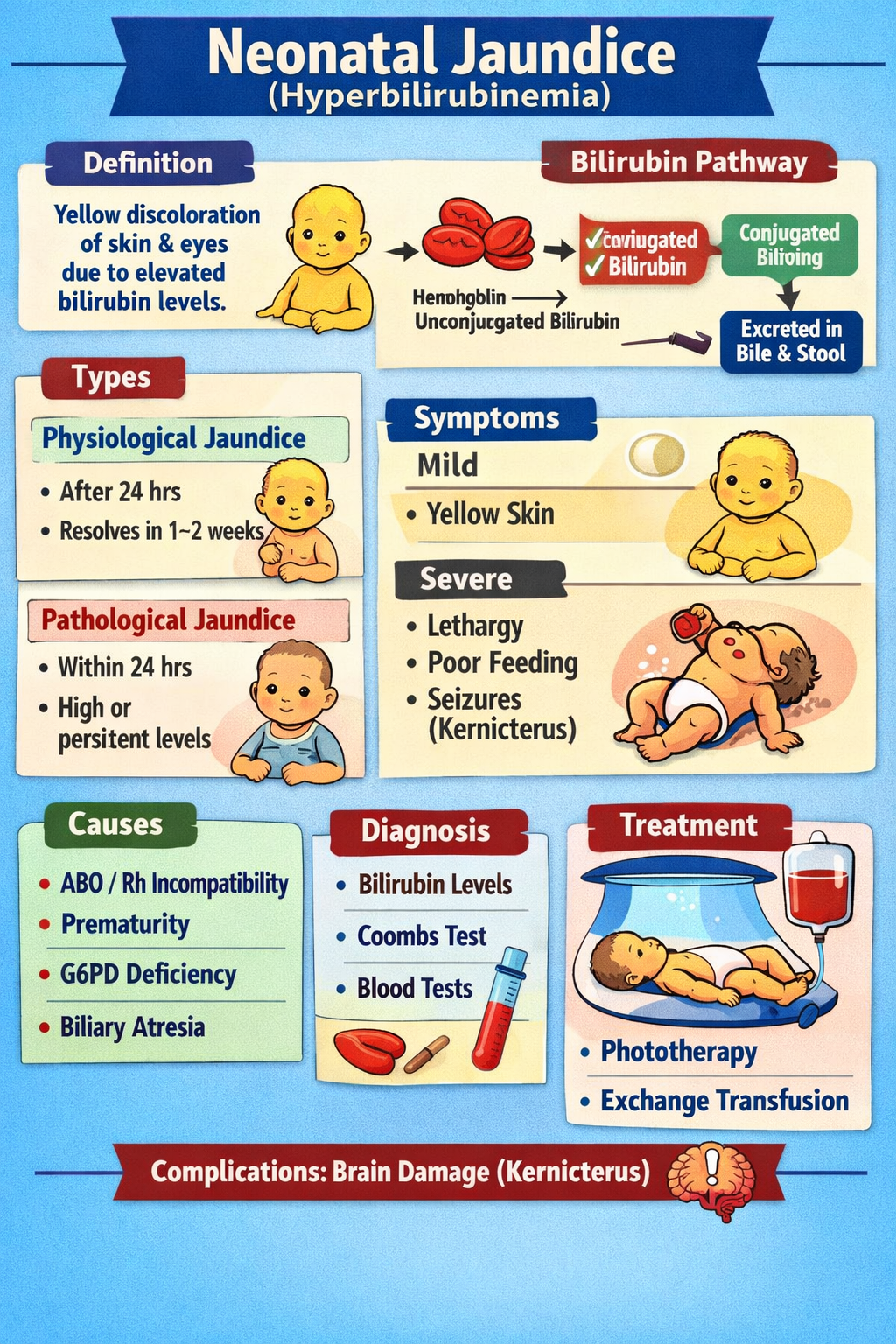
Neonatal jaundice is the yellow discoloration of a newborn’s skin and eyes caused by elevated bilirubin levels in the blood (hyperbilirubinemia).
Jaundice is common because newborns have increased red blood cell breakdown, immature liver enzymes for bilirubin conjugation, and increased enterohepatic circulation.
Physiological jaundice is normal jaundice appearing after 24 hours of life, peaking around day 3–5 in term infants, and resolving within 1–2 weeks without serious pathology.
Jaundice is pathological if it appears within the first 24 hours, rises rapidly, reaches very high bilirubin levels, persists beyond 2 weeks, or if conjugated bilirubin is elevated.
Early-onset jaundice is most commonly caused by hemolysis due to ABO incompatibility, Rh incompatibility, G6PD deficiency, or severe bruising/cephalhematoma.
Breastfeeding jaundice occurs early due to poor intake and dehydration, while breast milk jaundice occurs after day 7 due to substances in breast milk increasing enterohepatic circulation.
Danger signs include lethargy, poor feeding, hypotonia, high-pitched cry, arching (opisthotonus), seizures, and signs of acute bilirubin encephalopathy.
Kernicterus is chronic bilirubin encephalopathy caused by bilirubin deposition in the brain, leading to permanent neurological damage such as cerebral palsy and hearing loss.
Diagnosis is made by measuring total serum bilirubin (TSB), direct bilirubin levels, and evaluating risk factors with tests such as blood group and Coombs test.
A positive direct Coombs test indicates immune-mediated hemolysis, such as ABO or Rh incompatibility, causing pathological jaundice.
Conjugated hyperbilirubinemia is elevated direct bilirubin, always pathological, suggesting cholestasis or liver disease such as biliary atresia or neonatal hepatitis.
The main treatment is phototherapy, which converts unconjugated bilirubin into water-soluble forms that can be excreted without liver conjugation.
Phototherapy uses blue light (430–490 nm) to convert bilirubin into lumirubin and other isomers that are easily eliminated in bile and urine.
Side effects include dehydration, loose stools, skin rash, temperature instability, and rarely bronze baby syndrome in cholestasis.
Exchange transfusion is required when bilirubin reaches dangerous levels despite intensive phototherapy or when there are signs of acute bilirubin encephalopathy.
IVIG is used in immune hemolytic jaundice (Rh/ABO disease) to reduce hemolysis and decrease the need for exchange transfusion.
Prolonged jaundice lasts more than 14 days in term infants. Evaluation includes thyroid function tests, liver function tests, urine culture, and ruling out biliary atresia.
Biliary atresia causes obstructive cholestasis and requires early surgical intervention (Kasai procedure) to prevent liver failure.
Prevention includes early frequent feeding, bilirubin screening before discharge, identifying high-risk infants, and early follow-up after hospital discharge.
Urgent care is needed if jaundice appears within 24 hours, worsens rapidly, baby is lethargic or feeding poorly, has pale stools/dark urine, or shows neurological symptoms.