Medical Disclaimer: This is educational content only, not medical advice. Consult a licensed healthcare provider for diagnosis/treatment. Information based on sources like WHO/CDC guidelines (last reviewed: 2026-02-13).
This article is being expanded for more depth. Check back soon!
Neonatal Resuscitation Guide for Newborn Emergency Care
Frequently Asked Questions
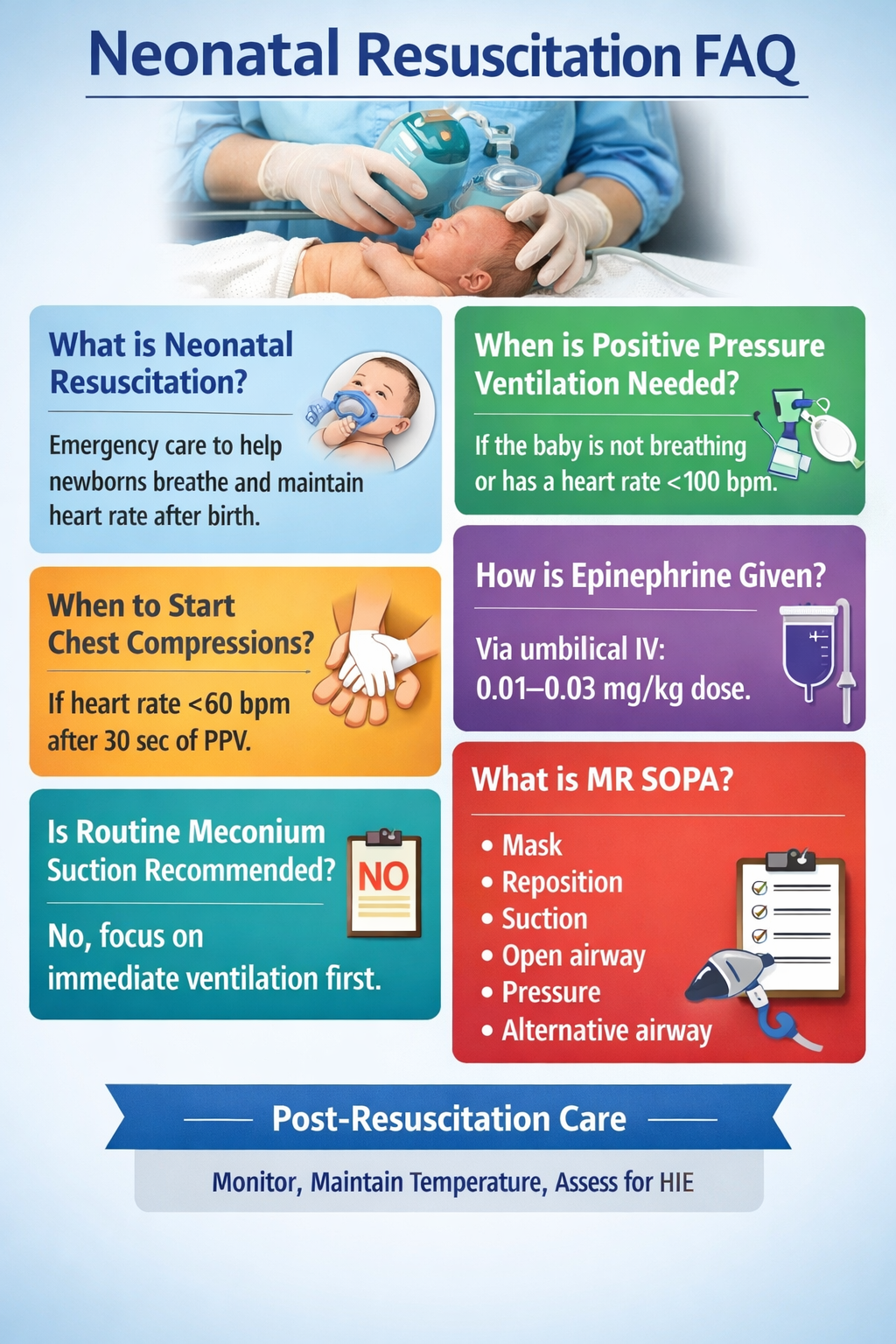
Neonatal resuscitation is a set of immediate interventions provided to a newborn after birth to establish effective breathing, adequate heart rate, and proper oxygenation when normal transition fails.
About 10% of newborns require some assistance at birth, while approximately 1% need extensive resuscitation including chest compressions or medications.
Effective ventilation is the most critical step, as most neonatal cardiac compromise is secondary to inadequate oxygenation and ventilation.
Positive pressure ventilation should be started if the newborn is apneic, gasping, or has a heart rate less than 100 beats per minute after initial stabilization.
Chest compressions are indicated when the heart rate remains below 60 beats per minute despite at least 30 seconds of effective positive pressure ventilation.
The recommended ratio is 3 compressions to 1 ventilation, resulting in 90 compressions and 30 breaths per minute.
Epinephrine is indicated if the heart rate remains below 60 beats per minute despite effective ventilation and coordinated chest compressions.
The preferred route is intravenous administration via an umbilical venous catheter, as it provides the fastest and most reliable effect.
Term newborns should be started on room air (21% oxygen), with oxygen concentration titrated based on pulse oximetry targets.
Preterm infants require careful temperature control, lower initial oxygen concentration (21–30%), gentle ventilation strategies, and may benefit from early CPAP.
No, routine suctioning is not recommended. Ventilation should be prioritized unless there is clear airway obstruction.
MR SOPA is a sequence of ventilation corrective steps: Mask adjustment, Reposition airway, Suction mouth and nose, Open mouth, Pressure increase, and Alternative airway.
Volume expansion is given when there is suspected hypovolemia due to blood loss, such as placental abruption or cord hemorrhage.
Normal oxygen saturation at 1 minute of life is approximately 60–65%, gradually increasing over the first 10 minutes.
Post-resuscitation care includes temperature control, glucose monitoring, cardiorespiratory monitoring, NICU observation, and evaluation for hypoxic ischemic encephalopathy.
Therapeutic hypothermia reduces brain injury and improves neurologic outcomes in eligible newborns with moderate to severe hypoxic ischemic encephalopathy.
Complications include hypoxic ischemic encephalopathy, pneumothorax, intracranial hemorrhage, pulmonary hemorrhage, and long-term neurodevelopmental impairment.
Neonatal cardiac compromise is primarily due to respiratory failure, so ventilation is emphasized more than compressions.
Prolonged absence of heart rate beyond 10 minutes despite optimal resuscitation is associated with very poor prognosis and requires individualized decision-making.
Essential equipment includes a radiant warmer, suction device, bag-mask ventilator, oxygen source with blender, pulse oximeter, airway devices, and emergency medications.